- Record: found
- Abstract: found
- Article: found
A State-of-the-Art Review on the Evolving Utility of Endoscopic Ultrasound in Liver Diseases Diagnosis
Read this article at
Abstract
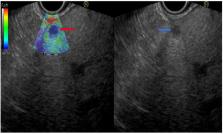
Liver diseases are amongst the most common diseases worldwide and manifest as a parenchymatic and/or biliary injury due to several causes as well as focal liver lesions, ranging from benign to malignant ones. The diagnosis of liver diseases is based mainly on biochemical and advanced imaging studies and, when required, on liver biopsy. Endoscopic ultrasound (EUS), which combines endoscopy and ultrasonography, is one of the main examination techniques used in gastroenterology as it is applied to evaluate abnormalities in the lumen of the upper and lower gastrointestinal tract and to define pancreatic and hepato-biliary features, often in chronic patients. Given its high spatial resolution and its proximity to the liver, EUS is gaining popularity in the diagnostic work up of liver diseases. This is a comprehensive overview of the current literature on the diagnostic indications for EUS use in patients with liver diseases. We performed a MEDLINE\PubMed and Embase search, and all articles that were relevant, after reviewing abstracts, were assessed and the full text was analyzed to extract data regarding technical success, diagnostic yield, bioptic characteristics, and complications rate. EUS-guided imaging and biopsy techniques in liver diseases have shown consistent favorable promising results among the reports through the literature, with an excellent diagnostic yield and safety profile, especially in the context of focal lesions and portal hypertension. The application of EUS in the diagnosis of liver diseases is a promising technique and should be considered as a first-line therapeutic option in selected cases.
Related collections
Most cited references39
- Record: found
- Abstract: found
- Article: not found
Assessment of morbidity and mortality associated with EUS-guided FNA: a systematic review.
- Record: found
- Abstract: found
- Article: not found
A meta-analysis of endoscopic ultrasound–fine-needle aspiration compared to endoscopic ultrasound–fine-needle biopsy: diagnostic yield and the value of onsite cytopathological assessment
- Record: found
- Abstract: found
- Article: not found