- Record: found
- Abstract: found
- Article: found
The influence of hypophosphatemia on outcomes of low- and high-intensity continuous renal replacement therapy in critically ill patients with acute kidney injury
Read this article at
Abstract
Background
The purpose of this study was to assess the role of hypophosphatemia in major clinical outcomes of patients treated with low- or high-intensity continuous renal replacement therapy (CRRT).
Methods
We performed a retrospective analysis of data collected from 492 patients. We divided patients into two CRRT groups based on treatment intensity (greater than or equal to or less than 40 mL/kg/hour of effluent generation) and measured serum phosphate level daily during CRRT.
Results
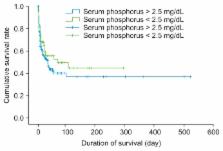
We obtained a total of 1,440 phosphate measurements on days 0, 1, and 2 and identified 39 patients (7.9%), 74 patients (15.0%), and 114 patients (23.1%) with hypophosphatemia on each of these respective days. In patients treated with low-intensity CRRT, there were 23 episodes of hypophosphatemia/1,000 patient days, compared with 83 episodes/1,000 patient days in patients who received high-intensity CRRT ( P < 0.01). Multiple Cox proportional hazards analysis showed that Acute Physiology and Chronic Health Evaluation (APACHE) III score, utilization of vasoactive drugs, and arterial pH on the second day of CRRT were significant predictors of mortality, while serum phosphate level was not a significant contributor to mortality.
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Hypophosphatemia: an update on its etiology and treatment.
- Record: found
- Abstract: found
- Article: not found
Recovery of renal function and survival after continuous renal replacement therapy during extracorporeal membrane oxygenation.
- Record: found
- Abstract: found
- Article: not found