- Record: found
- Abstract: found
- Article: found
Effectiveness of the Gold Standard Programme (GSP) for smoking cessation on smokers with and without a severe mental disorder: a Danish cohort study
Read this article at
Abstract
Objectives
We compared the effectiveness of an intensive smoking cessation intervention among smokers with and without a severe mental disorder (SMD) and identified factors associated with successful quitting. The main hypothesis was that smokers with an SMD would be less likely to stay continuously smoke-free for 6 months.
Setting
In all, 302 smoking cessation clinics in Denmark from municipal clinics, pharmacies, hospitals, midwives, primary care facilities and other private providers who reported data to the national Danish Smoking Cessation Database from 2006 to 2016 participated in this study.
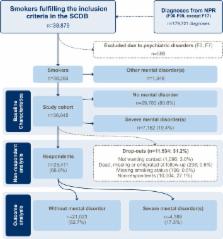
Participants
A total of 38 293 patients from the Danish Smoking Cessation Database. Patients with an SMD were identified by linking data to the Danish National Patient Register. Diagnoses of organic mental disorders (F0 chapter) or intellectual disabilities (F7 chapter) were not included. Smokers ≥18 years old who were attending a Gold Standard Programme (GSP) with planned follow-up were included. Smokers not wanting contact after 6 months were excluded.
Interventions
A comprehensive manual-based smoking cessation intervention comprising five meetings over a 6-week period (the GSP).
Results
In all, 69% of the participants participated in the follow-up after 6 months. The overall rate of successful quitting was high but significantly lower in SMD smokers (29% vs 38%; OR 0.74; 95% CI 0.68 to 0.80). Variables associated with successful quitting were compliance (defined as attending ≥75% of the planned meetings), older age and male gender as well as not being disadvantaged, heavy smoking or recommendation of intervention by health professionals.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery.

- Record: found
- Abstract: found
- Article: found
Smoking cessation in severe mental ill health: what works? an updated systematic review and meta-analysis
- Record: found
- Abstract: found
- Article: not found