- Record: found
- Abstract: found
- Article: found
Sentinel lymph node biopsy in squamous cell carcinoma of the head and neck: 10 years of experience Translated title: Il linfonodo sentinella nel carcinoma squamocellulare della testa e collo: 10 anni di esperienza
Read this article at
SUMMARY
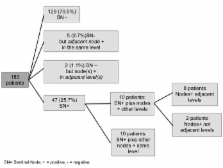
Sentinel node (SN) biopsy of head and neck cancer is still considered investigational, and agreement on the width of the surgical sampling has not yet been reached. From May 1999 to Dec 2009, 209 consecutive patients entered a prospective study: 61.7% had primary tumour of the oral cavity and 23.9% of the oropharynx. SN was not found in 26 patients. Based on these data and definitive histopathological analysis, we proposed six hypothetic scenarios to understand the percentage of neck recurrences following different treatments Among patients with identified SN, 54 cases were pN+: 47 in SN and 7 in a different node. Considering the six hypothetic scenarios: "only SN removal", "SN level dissection", "neck dissection from the tumour site to SN level", "selective neck dissection of three levels (SND)", "dissection from level I to IV" and "comprehensive I-V dissection", neck recurrences could be expected in 6.5%, 3.8%, 2.18%, 2.73%, 1.09% and 1.09% of cases, respectively. SN biopsy can be considered a useful tool to personalize the surgical approach to a N0 carcinoma. The minimum treatment of the neck is probably dissection of the levels between the primary tumour and the level containing the SN(s). Outside the framework of a clinical study, the best treatment can still be considered SND.
RIASSUNTO
La biopsia del linfonodo sentinella (SN) nel carcinoma squamocellulare della testa e collo è ancora considerata investigazionale e non è stata raggiunta unanimità su quanto ampio debba essere il prelievo da utilizzare. In questo studio prospettico, dal maggio 1999 al dicembre 2009, sono stati analizzati 209 pazienti consecutivi: 61,7% con tumore primitivo della cavità orale e 23,9% dell'orofaringe. Il SN non è stato identificato in 26 pazienti. Sulla base dei referti istopatologici definitivi, vengono creati sei scenari per ipotizzare quale sarebbe stato il tasso di ricorrenza nel collo se fossero stati impiegati i diversi trattamenti, più o meno invasivi. Dal totale di pazienti in cui è stato localizzato il SN, 54 casi sono stati pN+: 47 nel SN e 7 in un altro linfonodo. Considerando i sei scenari ipotetici: "rimozione solo SN", "dissezione livello contenente il SN", "svuotamento laterocervicale dal sito del tumore al livello del SN", "svuotamento selettivo di tre livelli (SND)", "svuotamento dei livelli I-IV" e "svuotamento dei livelli I-V", si sarebbero potute attendere rispettivamente 6,5%, 3,8%, 2,18%, 2,73%, 1,09% e 1,09% di recidive nel collo. La biopsia del SN può essere considerato uno strumento utile per personalizzare l'approccio chirurgico di un carcinoma squamocellulare N0 della testa e collo. Il trattamento minimo del collo è probabilmente la dissezione dei livelli fra il tumore primitivo ed il livello che contiene SN(s). Al di fuori di studi clinici, il miglior trattamento rimane lo SND.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
The influence of lymph node metastasis in the treatment of squamous cell carcinoma of the oral cavity, oropharynx, larynx, and hypopharynx: N0 versus N+.
- Record: found
- Abstract: found
- Article: not found
A meta-analysis of the randomized controlled trials on elective neck dissection versus therapeutic neck dissection in oral cavity cancers with clinically node-negative neck.
- Record: found
- Abstract: found
- Article: not found