- Record: found
- Abstract: found
- Article: found
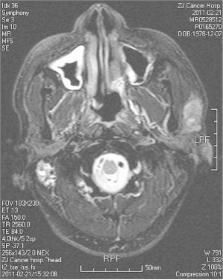
Metastasis of nasopharyngeal carcinoma to parotid lymph nodes: a retrospective study
Read this article at
Abstract
Background
Malignant parotid tumors are rare metastases originating from nasopharyngeal carcinoma (NPC). This study aimed to investigate the clinicopathological features and outcome of patients with metastasis of NPC to parotid lymph nodes after surgical therapy.
Methods
We enrolled 14 NPC patients who had metastatic disease to parotid lymph nodes after IMRT. They received surgical treatment by total parotidectomy with neck dissection, superficial parotidectomy with neck dissection, partial parotidectomy with neck dissection, total parotidectomy, or superficial parotidectomy. Their age, gender, histopathology, clinical findings, and treatment outcome were analyzed.
Results
After radiotherapy, parotid metastasis represented as uncontrolled disease in three cases and as recurrent disease in 11 cases. All the 14 patients received salvaged surgery successfully. Pathologic findings showed grade 3 in most patients. The follow-up ranged from 11 to 120 months and the overall three- and five-year survival was 49.5% and 37.1%, respectively.
Conclusions
Metastasis to parotid lymph nodes should be examined in NPC patients after IMRT. Resection of the inferior parotid lymph nodes is recommended for patients with cervical metastasis, and superficial or total parotidectomy and adjuvant therapy are recommended for intraparotid lymph node metastasis.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Cutaneous squamous cell carcinoma of the head and neck metastasizing to the parotid gland--a review of current recommendations.
- Record: found
- Abstract: found
- Article: not found
Occurrence of lymph node metastasis in early-stage parotid gland cancer.
- Record: found
- Abstract: found
- Article: not found