- Record: found
- Abstract: found
- Article: found
Prognostic accuracy of FIB‐4, NAFLD fibrosis score and APRI for NAFLD‐related events: A systematic review
Read this article at
Abstract
Background & Aims
Fibrosis is the strongest predictor for long‐term clinical outcomes among patients with non‐alcoholic fatty liver disease (NAFLD). There is growing interest in employing non‐invasive methods for risk stratification based on prognosis. FIB‐4, NFS and APRI are models commonly used for detecting fibrosis among NAFLD patients. We aimed to synthesize existing literature on the ability of these models in prognosticating NAFLD‐related events.
Methods
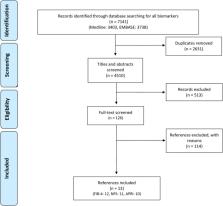
A sensitive search was conducted in two medical databases to retrieve studies evaluating the prognostic accuracy of FIB‐4, NFS and APRI among NAFLD patients. Target events were change in fibrosis, liver‐related event and mortality. Two reviewers independently performed reference screening, data extraction and quality assessment (QUAPAS tool).
Results
A total of 13 studies (FIB‐4:12, NFS: 11, APRI: 10), published between 2013 and 2019, were retrieved. All studies were conducted in a secondary or tertiary care setting, with follow‐up ranging from 1 to 20 years. All three markers showed consistently good prognostication of liver‐related events (AUC from 0.69 to 0.92). For mortality, FIB‐4 (AUC of 0.67‐0.82) and NFS (AUC of 0.70‐0.83) outperformed APRI (AUC of 0.52‐0.73) in all studies. All markers had inconsistent performance for predicting change in fibrosis stage.
Conclusions
FIB‐4, NFS, and APRI have demonstrated ability to risk stratify patients for liver‐related morbidity and mortality, with comparable performance to a liver biopsy, although more head‐to‐head studies are needed to validate this. More refined models to prognosticate NAFLD‐events may further enhance performance and clinical utility of non‐invasive markers.
Related collections
Most cited references45
- Record: found
- Abstract: found
- Article: not found
QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies.
- Record: found
- Abstract: found
- Article: not found
Design and validation of a histological scoring system for nonalcoholic fatty liver disease.
- Record: found
- Abstract: found
- Article: not found