- Record: found
- Abstract: found
- Article: found
Performance of pfHRP2 versus pLDH antigen rapid diagnostic tests for the detection of Plasmodium falciparum: a systematic review and meta-analysis
Read this article at
Abstract
Introduction
There have been many inconsistent reports about the performance of histidine-rich protein 2 (HRP2) and lactate dehydrogenase (LDH) antigens as rapid diagnostic tests (RDTs) for the diagnosis of past Plasmodium falciparum infections. This meta-analysis was performed to determine the performance of pfHRP2 versus pLDH antigen RDTs in the detection of P. falciparum.
Material and methods
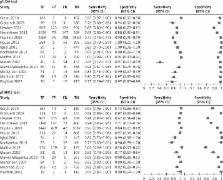
After a systematic review of related studies, Meta-DiSc 1.4 software was used to calculate the pooled sensitivity, specificity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and diagnostic odds ratio (DOR). Forest plots and summary receiver operating characteristic curve (SROC) analysis were used to summarize the overall test performance.
Results
Fourteen studies which met the inclusion criteria were included in the meta-analysis. The summary performances for pfHRP2- and pLDH-based tests in the diagnosis of P. falciparum infections were as follows: pooled sensitivity, 96.3% (95.8–96.7%) vs. 82.6% (81.7–83.5%); specificity, 86.1% (85.3–86.8%) vs. 95.9% (95.4–96.3%); diagnostic odds ratio (DOR), 243.31 (97.679–606.08) vs. 230.59 (114.98–462.42); and area under ROCs, 0.9822 versus 0.9849 (all p < 0.001).
Conclusions
The two RDTs performed satisfactorily for the diagnosis of P. falciparum, but the pLDH tests had higher specificity, whereas the pfHRP2 tests had better sensitivity. The pfHRP2 tests had slightly greater accuracy compared to the pLDH tests. A combination of both antigens might be a more reliable approach for the diagnosis of malaria.
Related collections
Most cited references22

- Record: found
- Abstract: found
- Article: found
Systematic review and meta-analysis: rapid diagnostic tests versus placental histology, microscopy and PCR for malaria in pregnant women
- Record: found
- Abstract: found
- Article: not found
Meta-analysis: accuracy of rapid tests for malaria in travelers returning from endemic areas.
- Record: found
- Abstract: found
- Article: not found