- Record: found
- Abstract: found
- Article: not found
Very late-onset neuromyelitis optica spectrum disorder beyond the age of 75
Read this article at
Abstract
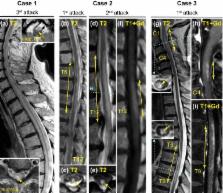
Aquaporin-4 antibody (AQP4-Ab)-positive neuromyelitis optica spectrum disorder (NMOSD) is a rare but often severe autoimmune disease with median onset around 40 years of age. We report characteristics of three very-late-onset NMOSD (including complete NMO) patients >75 years of age, in whom this diagnosis initially seemed unlikely because of their age and age-associated concomitant diseases, and briefly review the literature. All three patients, aged 79, 82 and 88 years, presented with a spinal cord syndrome as the first clinical manifestation of AQP4-Ab-positive NMOSD. They all had severe relapses unless immunosuppressive therapy was initiated, and one untreated patient died of a fatal NMOSD course. Two patients developed side effects of immunosuppression. We conclude that a first manifestation of NMOSD should be considered even in patients beyond the age of 75 years with a compatible syndrome, especially longitudinally extensive myelitis. Early diagnosis and treatment are feasible and highly relevant. Special attention is warranted in the elderly to recognize adverse effects of immunosuppressive therapies as early as possible.
Related collections
Most cited references16

- Record: found
- Abstract: found
- Article: found
Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: A multicentre study of 175 patients
- Record: found
- Abstract: found
- Article: not found
Seroprevalence of autoantibodies against brain antigens in health and disease.
- Record: found
- Abstract: found
- Article: not found
