- Record: found
- Abstract: found
- Article: found
Assessment of educational intervention and Acupressure during labor on the mother's anxiety level and arterial oxygen pressure of the umbilical cord of infants (PO2). A randomized controlled clinical Trial
Read this article at
Abstract
BACKGROUND:
Natural delivery is distressing, and the mother's anxiety in this condition can have negative impacts on the fetus, mother, and the delivery process. Hence, many women tend to use pharmacological or nonpharmacological methods for reduction of labor stress and anxiety. The aim was to assess the effect of supportive care and acupressure during labor on the mother's anxiety level and arterial oxygen pressure of the umbilical cord of infants.
MATERIALS AND METHODS:
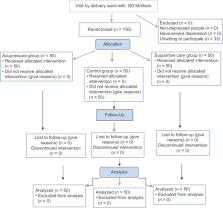
This performed on 150 pregnant women were randomly assigned to two interventions and a control group in the delivery ward of the selected educational center of Shiraz University of Medical Sciences (Shoushtari Hospital) in Iran. Mothers’ anxiety scores before (beginning of the active stage of labor) and after intervention (the end of the first stage of labor) were measured using Spielberger's questionnaire. Then, infants’ cord blood samples for arterial blood gas and hematologic analyses were sent to the hospital's laboratory. After all, the data with SPSS version 16 and using Pearson's correlation coefficient, one-way ANOVA, were analyzed.
RESULTS:
The mean of anxiety score in the control group was 21.1% and in the supportive group and the acupressure group, respectively, decreased by 37.5% and 34.8%, respectively ( P < 0.001). The mean of PO 2 was also reported in the maternal supportive, acupressure, and control groups, 40.4 ± 8.8, 27.4 ± 2.8, and 18.1 ± 3.7, respectively. Additionally, a significant correlation was found between mothers’ anxiety scores after the intervention and the mean of PO 2 ( P = 0.014).
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: not found
4 million neonatal deaths: when? Where? Why?
- Record: found
- Abstract: found
- Article: not found
Placental corticotropin-releasing hormone (CRH), spontaneous preterm birth, and fetal growth restriction: a prospective investigation.
- Record: found
- Abstract: found
- Article: not found