- Record: found
- Abstract: found
- Article: found
Trends in chloroquine resistance marker, Pfcrt-K76T mutation ten years after chloroquine withdrawal in Tanzania
Read this article at
Abstract
Background
Plasmodium falciparum resistance to anti-malarial drugs remains a major obstacle to the control of malaria. In 2001 Tanzania replaced chloroquine (CQ) with sulphadoxine-pyrimethamine (SP) as first-line drug, which in turn was replaced by artemisinin combination therapy in 2006. SP has however, continued to be used in intermittent preventive treatment of malaria in pregnancy (IPTp) despite reports of high levels of resistance to SP due to the lack of alternatives to SP for IPTp. Recent reports have indicated recovery of CQ-susceptibility in Malawi, Kenya, Mozambique, and Tanzania based on the prevalence of wild types at codon 76 of the Pfcrt gene in indigenous P. falciparum populations. The current prevalence of this Pfcrt-76 CQ resistance marker from six regions of Tanzania mainland is hereby reported.
Methods
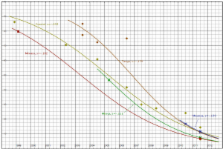
DNA extracted from filter-paper dried blood spots and rapid diagnostics kit strips collected from finger-prick blood were used to genotype the Pfcrt-76 resistance marker using PCR-RFLP. Data from previously published studies were used to generate CQ susceptibility recovery trends using logistic regression model.
Results
Seven hundred and forty one (741) samples were genotyped. The current frequency of the CQ-susceptible Pfcrt-K76 was above 92% and did not differ between regions in Tanzania ( χ2 = 2.37; p = 0.795). The K76 allelic prevalence was between 85.7 and 93% in regions ( χ2 = 7.88, p = 0.163). The CQ resistance recovery trends showed regional variability that may be caused by differences in malaria transmission intensity, but overall the trends converge as the susceptibility levels in all regions approach >90%.
Conclusions
CQ withdrawal in Tanzania has resulted into >90% recovery of susceptibility in ten years of withdrawal. These findings are in support of the search for CQ-based combination drugs as a possible future alternative to SP for IPTp in places where full recovery of CQ-susceptibility will be evident.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
Reemergence of chloroquine-sensitive Plasmodium falciparum malaria after cessation of chloroquine use in Malawi.
- Record: found
- Abstract: found
- Article: not found