- Record: found
- Abstract: found
- Article: found
Ultrasound-guided erector spinae plane block for postoperative short-term outcomes in lumbar spine surgery: A meta-analysis and systematic review
Read this article at
Background:
Patients undergoing lumbar spine surgery usually suffer from moderate to severe acute pain. Erector spinae plane block (ESPB) has been applied to relieve acute pain in various surgeries and improve postoperative outcomes. This study aimed to further identify the efficacy and safety of erector spinae plane block in patients undergoing lumbar spine surgery. This study also evaluates the outcomes of the erector spinae plane block compared with other regional blocks.
Methods:
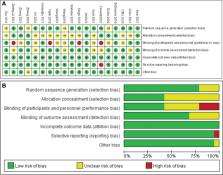
We searched PubMed, Web of Science, Cochrane library, Embase, and CINAHL databases to identify all randomized controlled trials evaluating the effects of ESPB on postoperative pain after lumbar spine surgery. The primary outcome is postoperative total opioid consumption in 24 hours. The secondary outcomes are postoperative pain scores, intraoperative opioid consumption, time to first rescue analgesia, number of patients requiring rescue analgesia, first time to ambulation after surgery, length of hospital stay, patients’ satisfaction score, and postoperative side effects such as postoperative nausea and vomiting, itching.
Results:
A total of 19 randomized controlled trials are included in the final analysis. Compared with no/sham block, ultrasound-guided erector spinae plane block can decrease perioperative opioid consumption including intraoperative opioid consumption: standardized mean difference (SMD) = −3.04, 95% confidence interval (CI) (−3.99, −2.09), P < .01, and opioid consumption postoperatively: (SMD = −2.80, 95% CI [−3.61, −2.00], P < .01); reduce postoperative pain at 2, 6, 12, 24, and 48 hours both at rest and movement; meanwhile shorten time to hospital length of stay: (SMD = −1.01, 95% CI [−1.72, 0.30], P = .006), decrease postoperative nausea and vomiting (RR = 0.35, 95% CI [0.27, 0.46], P < .00001), and improve patient satisfaction (SMD = −2.03, 95% CI [−0.96, 3.11], P = .0002). But ultrasound-guided ESPB doesn’t shorten the time to ambulation after surgery (SMD = −0.56, 95% CI [−1.21, 0.08], P = .09). Additionally, ESPB is not superior to other regional blocks (e.g., thoracolumbar interfascial plane/midtransverse process to pleura block).
Conclusion:
This meta-analysis demonstrates that ultrasound-guided ESPB can provide effective postoperative analgesia in patients undergoing lumbar spine surgery and improve postoperative outcomes, and it deserves to be recommended as an analgesic adjunct in patients undergoing lumbar spine surgeries.
Related collections
Most cited references56

- Record: found
- Abstract: found
- Article: found
The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials
- Record: found
- Abstract: found
- Article: not found
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement

- Record: found
- Abstract: found
- Article: found