- Record: found
- Abstract: found
- Article: found
The relationship between childhood trauma, dopamine release and dexamphetamine-induced positive psychotic symptoms: a [ 11C]-(+)-PHNO PET study
Abstract
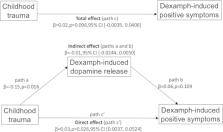
Childhood trauma is a risk factor for psychosis. Amphetamine increases synaptic striatal dopamine levels and can induce positive psychotic symptoms in healthy individuals and patients with schizophrenia. Socio-developmental hypotheses of psychosis propose that childhood trauma and other environmental risk factors sensitize the dopamine system to increase the risk of psychotic symptoms, but this remains to be tested in humans. We used [ 11C]-(+)-PHNO positron emission tomography to measure striatal dopamine-2/3 receptor (D 2/3R) availability and ventral striatal dexamphetamine-induced dopamine release in healthy participants ( n = 24). The relationships between dexamphetamine-induced dopamine release, dexamphetamine-induced positive psychotic symptoms using the Positive and Negative Syndrome Scale (PANSS), and childhood trauma using the Childhood Trauma Questionnaire (CTQ) were assessed using linear regression and mediation analyses, with childhood trauma as the independent variable, dexamphetamine-induced dopamine release as the mediator variable, and dexamphetamine-induced symptoms as the dependent variable. There was a significant interaction between childhood trauma and ventral striatal dopamine release in predicting dexamphetamine-induced positive psychotic symptoms (standardized β = 1.83, p = 0.003), but a mediation analysis was not significant (standardized β = −0.18, p = 0.158). There were no significant effects of dopamine release and childhood trauma on change in negative ( p = 0.280) or general PANSS symptoms ( p = 0.061), and there was no relationship between ventral striatal baseline D 2/3R availability and positive symptoms ( p = 0.368). This indicates childhood trauma and dopamine release interact to influence the induction of positive psychotic symptoms. This is not consistent with a simple sensitization hypothesis, but suggests that childhood trauma moderates the cognitive response to dopamine release to make psychotic experiences more likely.
Related collections
Most cited references70
- Record: found
- Abstract: found
- Article: not found
The environment and schizophrenia.
- Record: found
- Abstract: found
- Article: not found