- Record: found
- Abstract: found
- Article: found
Preimplantation Genetic Testing for Aneuploidy Could Not Improve Cumulative Live Birth Rate Among 705 Couples with Unexplained Recurrent Implantation Failure
Read this article at
Abstract
Objective
We evaluate whether next-generation sequencing (NGS)-based preimplantation genetic testing for aneuploidy (PGT-A) improves the cumulative pregnancy outcomes of patients with unexplained recurrent implantation failure (uRIF) as compared to conventional in vitro fertilization or intracytoplasmic sperm injection (IVF/ICSI).
Patients and Methods
This was a retrospective cohort study (2015–2022). A total of 705 couples diagnosed with uRIF were included in the study. 229 women transferred blastocysts based on morphological grading (IVF/ICSI) and 476 couples opted for PGT-A to screen blastocysts by NGS. Women were further stratified according to age at retrieval (<38 years and ≥38 years). The primary outcome was the cumulative live-birth rate after all the embryos were transferred in a single oocyte retrieval or until achieving a live birth. Confounders were adjusted using binary logistic regression models.
Results
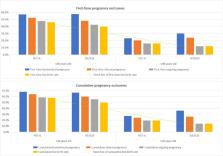
Cumulative live-birth rate was similar between the IVF/ICSI group and the PGT-A group after stratified by age: IVF/ICSI vs PGT-A in the <38 years subgroup (49.7% vs 57.7%, adjusted OR (95% CI) = 1.25 (0.84–1.84), P = 0.270) and in the ≥38 years subgroup (14.0% vs 19.5%, adjusted OR (95% CI) = 1.09 (0.41–2.92), P = 0.866), respectively. Nonetheless, the PGT group had a lower first-time biochemical pregnancy loss rate (17.0% vs 8.7%, P = 0.034) and a higher cumulative good birth outcome rate (35.2% vs 46.4%, P = 0.014) than the IVF/ICSI group in the <38 years subgroup. Other pregnancy outcomes after the initial embryo transfer and multiple transfers following a single oocyte retrieval were all similar between groups.
Conclusion
Our results showed no evidence of favorable effects of PGT-A treatment on improving the cumulative live birth rate in uRIF couples regardless of maternal age. Use of PGT-A in the <38 years uRIF patients would help to decrease the first-time biochemical pregnancy loss and increase the cumulative good birth outcome.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening.
- Record: found
- Abstract: found
- Article: not found
Frozen versus fresh single blastocyst transfer in ovulatory women: a multicentre, randomised controlled trial
- Record: found
- Abstract: found
- Article: not found