- Record: found
- Abstract: found
- Article: found
Inter-rater reliability of the Berg Balance Scale, 30 s chair stand test and 6 m walking test, and construct validity of the Berg Balance Scale in nursing home residents with mild-to-moderate dementia
Read this article at
Abstract
Objective
When testing physical function, patients must be alert and have the capacity to understand and respond to instructions. Patients with dementia may have difficulties fulfilling these requirements and, therefore, the reliability of the measures may be compromised. We aimed to assess the inter-rater reliability between pairs of observers independently rating the participant in the Berg Balance Scale (BBS), 30 s chair stand test (CST) and 6 m walking test. We also wanted to investigate the internal consistency of the BBS.
Setting
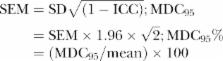
We included 33 nursing home patients with a mild-to-moderate degree of dementia and tested them once with two evaluators present. One evaluator gave instructions and both evaluators scored the patients’ performance. Weighted κ, intraclass correlation coefficient (ICC) model 2.1 with 95% CIs and minimal detectable change (MDC) were used to measure inter-rater reliability. Cronbach's α was calculated to evaluate the internal consistency of the BBS sum score.
Results
The mean values of the BBS scored by the two evaluators were 38±13.7 and 38.0±13.8, respectively. Weighted κ scores for the BBS items varied from 0.83 to 1.0. ICC for the BBS's sum score was 0.99, and the MDC was 2.7% and 7%, respectively. The Cronbach’s α of the BBS's sum score was 0.9. The ICC of the CST and 6 m walking test was 1 and 0.97, respectively. The MDC on the 6 m walking test was 0.08% and 15.2%, respectively.
Conclusions
The results reveal an excellent relative inter-rater reliability of the BBS, CST and 6 m walking test as well as high internal consistency for the BBS in a population of nursing home residents with mild-to-moderate dementia. The absolute reliability was 2.7 on the BBS and 0.08 on the 6 m walking test.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Physical performance measures in the clinical setting.
- Record: found
- Abstract: found
- Article: not found