- Record: found
- Abstract: found
- Article: found
Using Relative and Absolute Measures for Socioeconomic Inequalities in Health: Experiences from a Retrospective Cohort Study on COVID-19
Read this article at
Abstract
Background:
One approach to reducing the burden of diseases can be to identify socioeconomically vulnerable groups. We aimed to estimate the socioeconomic inequality of in-hospital deaths using relative and absolute indices of socioeconomic inequality.
Methods:
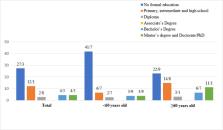
In this retrospective cohort study on Covid-19 patients; age, gender, marital status, education level, date of admission, diagnostic method, and final condition were measured. Socioeconomic inequality in inhospital death was assessed using three approaches. We used the relative index of inequality (RII) to measure relative inequality. We used two approaches to evaluate absolute inequality: the slope index of inequality (SII) and the concentration index (ci).
Results:
Overall, 587 patients’ data were collected and 42 (7.2%) of these patients died in the hospital. There were statistically significant differences between the case-fatality rates of different levels of education ( P<0.001). In addition, all the inequality indices showed that the distribution of COVID-19-related deaths was higher among the lower education levels. Accordingly, after controlling the effect of age, gender, and comorbidities the RII indicated that the case fatality rate in the lowest education level was 9.42 (95% CI: 2.23 to 39.01, P<0.001) times compared to the case fatality rate in the highest level of education.
Conclusion:
The results of all three approaches indicate considerable education inequality in CFR in favor of groups of high education levels. These results can improve the prioritization and impact of public health interventions, including prevention and diagnosis of Covid-19 in favor of vulnerable groups.
Related collections
Most cited references39

- Record: found
- Abstract: found
- Article: found
OpenSAFELY: factors associated with COVID-19 death in 17 million patients
- Record: found
- Abstract: found
- Article: not found
Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China

- Record: found
- Abstract: found
- Article: found