- Record: found
- Abstract: found
- Article: found
Predictors and triggers of incivility within healthcare teams: a systematic review of the literature
Read this article at
Abstract
Objectives
To explore predictors and triggers of incivility in medical teams, defined as behaviours that violate norms of respect but whose intent to harm is ambiguous.
Data sources
Database searches according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline in Medline, CINHAL, PsychInfo, Web of Science and Embase up to January 2020.
Eligibility criteria
Original empirical quantitative and qualitative studies focusing on predictors and triggers of incivilities in hospital healthcare teams, excluding psychiatric care.
Data extraction and synthesis
Of the 1397 publications screened, 53 were included (44 quantitative and 9 qualitative studies); publication date ranged from 2002 to January 2020.
Results
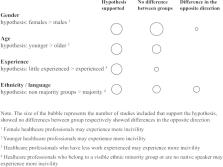
Based on the Medical Education Research Study Quality Instrument (MERSQI) scores, the quality of the quantitative studies were relatively low overall (mean MERSQI score of 9.93), but quality of studies increased with publication year (r=0.52; p<0.001). Initiators of incivility were consistently described as having a difficult personality, yet few studies investigated their other characteristics and motivations. Results were mostly inconsistent regarding individual characteristics of targets of incivilities (eg, age, gender, ethnicity), but less experienced healthcare professionals were more exposed to incivility. In most studies, participants reported experiencing incivilities mainly within their own professional discipline (eg, nurse to nurse) rather than across disciplines (eg, physician to nurse). Evidence of specific medical specialties particularly affected by incivility was poor, with surgery as one of the most cited uncivil specialties. Finally, situational and cultural predictors of higher incivility levels included high workload, communication or coordination issues, patient safety concerns, lack of support and poor leadership.
Conclusions
Although a wide range of predictors and triggers of incivilities are reported in the literature, identifying characteristics of initiators and the targets of incivilities yielded inconsistent results. The use of diverse and high-quality methods is needed to explore the dynamic nature of situational and cultural triggers of incivility.
Related collections
Most cited references79
- Record: found
- Abstract: not found
- Article: not found
A Qualitative Analysis of Conflict Types and Dimensions in Organizational Groups
- Record: found
- Abstract: not found
- Article: not found
Tit for Tat? The Spiraling Effect of Incivility in the Workplace
- Record: found
- Abstract: found
- Article: not found