- Record: found
- Abstract: found
- Article: found
Current Practice in Obstetric Anesthesia and Analgesia in Public Hospitals of Greece: A 2016 National Survey
Read this article at
Abstract
Aims:
This descriptive survey was to evaluate the use of regional anesthesia in obstetrics in Greek public hospitals.
Methods:
The survey was conducted between March and August 2016. A structured questionnaire was sent to 50 anesthesia departments in Greek public hospitals with obstetric units.
Results:
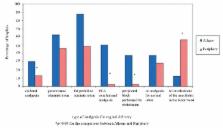
The response rate was 94%. Data corresponding to 9475 cesarean and 8155 vaginal deliveries were collected. Regional anesthesia was used in 69.2% of all cesareans, with single shot spinal being the most popular (44.3% of all cesareans). Combined spinal-epidural anesthesia was used in 18.1% of all cesareans (35.1% in hospitals of Athens versus 7.9% outside Athens, p<0.001). Post-cesarean analgesia was applied with simple analgesics and systematic opioids (78.6%). Long-acting spinal opioids were rarely used (4.4% of spinal and spinal/epidurals). Labor epidural analgesia was applied in 19.1% of all vaginal deliveries (30.3% in Athens versus 13.1% outside Athens, p<0.001). Paracetamol and pethidine represented the standard labor analgesics in 48.9% and 55.3% of all hospitals. Intravenous remifentanil was used in 10.6% of hospitals (50% in Athens versus 2.5% outside Athens, p=0.002). In 48.9% of hospitals, mainly outside Athens, the anesthesiologists did not get involved in labor analgesia.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
PDPH is a common complication of neuraxial blockade in parturients: a meta-analysis of obstetrical studies.
- Record: found
- Abstract: found
- Article: not found