- Record: found
- Abstract: found
- Article: not found
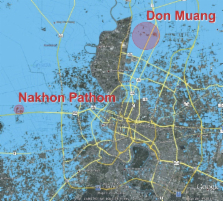
Leptospira Species in Floodwater during the 2011 Floods in the Bangkok Metropolitan Region, Thailand
Abstract
Floodwater samples ( N = 110) collected during the 2011 Bangkok floods were tested for Leptospira using culture and polymerase chain reaction (PCR); 65 samples were PCR-positive for putatively non-pathogenic Leptospira species, 1 sample contained a putatively pathogenic Leptospira, and 6 samples contained Leptospira clustering phylogenetically with the intermediate group. The low prevalence of pathogenic and intermediate Leptospira in floodwater was consistent with the low number of human leptospirosis cases reported to the Bureau of Epidemiology in Thailand. This study provides baseline information on environmental Leptospira in Bangkok together with a set of laboratory tests that could be readily deployed in the event of future flooding.
Related collections
Most cited references4
- Record: found
- Abstract: found
- Article: not found
Epidemic leptospirosis associated with pulmonary hemorrhage-Nicaragua, 1995.
- Record: found
- Abstract: found
- Article: not found
Outbreak of Leptospirosis after Flood, the Philippines, 2009

- Record: found
- Abstract: found
- Article: found
Molecular detection and speciation of pathogenic Leptospira spp. in blood from patients with culture-negative leptospirosis
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.