- Record: found
- Abstract: found
- Article: found
Transplant Center Variability in Disparities for African-American Kidney Transplant Recipients
Read this article at
Abstract
Background
Disparities research has traditionally focused on patient-level variables to ascertain predominant risk factors driving differences in outcomes for African-American (AA) kidney transplant recipients. Our objectives were to determine the magnitude and impact of transplant center variability for graft outcome disparities.
Material/Methods
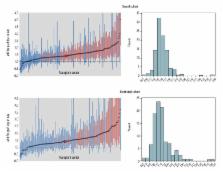
This was a retrospective cohort study analyzing 25 years of U.S. national transplant registry data at both the patient and center levels using univariate descriptive statistics and multivariable modeling.
Results
A total of 257,024 recipients from 191 centers were analyzed; AAs represented 31.1% of recipients. After adjusting for baseline characteristics, AAs had 42% higher risk of graft loss (aHR 1.42, 95% CI 1.39 to 1.45; p<0.001). Center variability for graft outcome disparities in AAs was significant (race*center interaction term p<0.05), with the aHRs ranging from 0.5 to 4.9; 46% of centers demonstrated a non-statistically significant disparity (aHR p>0.05) and 25% of centers had a large AA disparity (aHR >1.75). In a more recent transplant time period (2000–14), overall racial disparities decreased but center-level disparities increased in variability. Center-level factors significantly associated with increasing disparity included higher acute rejection rates, fewer transplants per year, longer length of stay, lower use of calcineurin inhibitors (CNI), and lower living donor rates.
Conclusions
There is evidence of significant center-level variability in graft outcome disparities for AA kidney recipients. Further, there appears to be a number of center-level factors associated with this variability, including acute rejection rates, CNI use, number of transplants per year, and, in recent years, low living donor rates.
Related collections
Most cited references28
- Record: found
- Abstract: found
- Article: not found
Disparities in health care are driven by where minority patients seek care: examination of the hospital quality alliance measures.
- Record: found
- Abstract: found
- Article: not found
Hospital-level racial disparities in acute myocardial infarction treatment and outcomes.
- Record: found
- Abstract: found
- Article: not found