- Record: found
- Abstract: found
- Article: found
Aortotracheal fistula after slide tracheoplasty in a patient with dextrocardia, left pulmonary artery sling and tracheal stenosis: a case report
Read this article at
Abstract
Background
Aortotracheal fistula (ATF) is an uncommon and fatal complication of tracheal or aortic surgery, especially among pediatric patients.
Case presentation
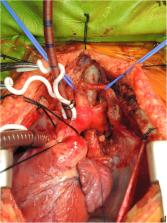
We reported a case in a 1-year-old boy with dextrocardia, left pulmonary artery sling and long segment tracheal stenosis. He received slide tracheoplasty at 9 months of age and had post-operative refractory granulation at distal trachea status post repeated balloon dilatation and laser vaporization. Episodes of hemoptysis occurred on post-operative day 81. Bronchoscopy revealed a pulsating pseudoaneurysm at lower trachea which ruptured during the procedure
Urgent surgical repair under cardiopulmonary bypass with deep hypothermic circulatory arrest was done. No recurrent bleeding or significant neurologic deficits noticed at a 4-month follow-up.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Postoperative aortic fistulas into the airways: etiology, pathogenesis, presentation, diagnosis, and management.
- Record: found
- Abstract: found
- Article: not found
Aorto-oesophageal and aortobronchial fistulae following thoracic endovascular aortic repair: a national survey.
- Record: found
- Abstract: not found
- Article: not found