- Record: found
- Abstract: found
- Article: found
ED 90 of epidural esketamine with 0.075% ropivacaine for labor analgesia in nulliparous parturients: a prospective, randomized and dose-finding study
Read this article at
Abstract
Background: Because it has been reported that racemic ketamine had a local anesthetic-sparing effect when used for epidural analgesia this would suggest the likelihood of a potential advantage (less pruritus) over opioid drugs. Esketamine has greater analgesic efficacy than racemic ketamine, but the optimum dosage regimen for epidural use is undetermined. The aim of this study was to determine the ED 90 of epidural esketamine when coadministered with 0.075% ropivacaine for labor analgesia.
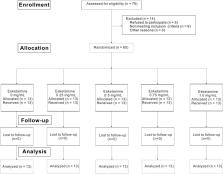
Methods: A total of 65 laboring nulliparous patients were enrolled in this study from 16 March 2022 to 15 October 2022. The patients were randomly assigned to receive 0, 0.25, 0.5, 0.75 or 1.0 mg/mL esketamine with 0.075% ropivacaine epidurally. An effective response to the epidural loading dose was defined as numerical rating scale pain score ≤3 at 30 min after the end of the epidural loading dose (10 mL of the ropivacaine 0.075% solution with the added esketamine). The ED 90 of epidural esketamine coadministered with 0.075% ropivacaine with 95% confidence intervals for labor analgesia was determined using probit regression. Secondary outcomes and side effects were recorded.
Results: The estimated value of ED 90 with 95% CIs for epidural esketamine with 0.075% ropivacaine was 0.983 (0.704–2.468) mg/mL. The characteristics of sensory and motor block, consumption of ropivacaine per hour, duration of first or second stage, Apgar scores did not differ among the five groups. The incidence of mild dizziness in Group esketamine 1.0 mg/mL was significantly higher than that in other groups ( p < 0.05). No statistical differences were found in other side effects among groups.
Conclusion: The ED 90 value of epidural esketamine coadministered with 0.075% ropivacaine for labor analgesia in nulliparous parturients was about 1.0 mg/mL. Furthermore, our results suggested that epidural esketamine would cause dose-dependent mild dizziness especially at doses up to 1.0 mg/mL. As a single epidural additive, esketamine may not be suitable for labor analgesia. Future studies may investigate the appropriate dosage of esketamine at slightly higher concentrations of local anesthetics or larger initial volume of analgesia, or explore other potential advantages of esketamine.
Clinical Trial Registration: ( https://www.chictr.org.cn/bin/project/edit?pid=159764), identifier (ChiCTR2200057662).
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Cognitive impairment after small-dose ketamine isomers in comparison to equianalgesic racemic ketamine in human volunteers.
- Record: found
- Abstract: found
- Article: not found
Relative analgesic potencies of ropivacaine and bupivacaine for epidural analgesia in labor: implications for therapeutic indexes.
- Record: found
- Abstract: found
- Article: not found