- Record: found
- Abstract: found
- Article: found
Proposed refined diagnostic criteria and classification of eosinophil disorders and related syndromes
Read this article at
Abstract
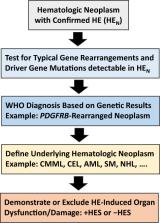
Eosinophilia and eosinophil activation are recurrent features in various reactive states and certain hematologic malignancies. In patients with hypereosinophilia (HE), HE‐induced organ damage is often encountered and may lead to the diagnosis of a hypereosinophilic syndrome (HES). A number of known mechanisms and etiologies contribute to the development of HE and HES. Based on these etiologies and the origin of eosinophils, HE and HES are divided into primary forms where eosinophils are clonal cells, reactive forms where an underlying reactive or neoplastic condition is detected and eosinophils are considered to be “non‐clonal” cells, and idiopathic HE and HES in which neither a clonal nor a reactive underlying pathology is detected. Since 2012, this classification and the related criteria have been widely accepted and regarded as standard. However, during the past few years, new developments in the field and an increasing number of markers and targets have created a need to update these criteria and the classification of HE and HES. To address this challenge, a Working Conference on eosinophil disorders was organized in 2021. In this conference, a panel of experts representing the relevant fields, including allergy, dermatology, hematology, immunology, laboratory medicine, and pathology, met and discussed new markers and concepts as well as refinements in definitions, criteria and classifications of HE and HES. The outcomes of this conference are presented in this article and should assist in the diagnosis and management of patients with HE and HES in daily practice and in the preparation and conduct of clinical trials.
Related collections
Most cited references72
- Record: found
- Abstract: found
- Article: found
The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Myeloid and Histiocytic/Dendritic Neoplasms
- Record: found
- Abstract: found
- Article: not found
Contemporary consensus proposal on criteria and classification of eosinophilic disorders and related syndromes.
- Record: found
- Abstract: found
- Article: not found
A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome.
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.