- Record: found
- Abstract: found
- Article: found
Recognizing the emergency department’s role in oncologic care: a review of the literature on unplanned acute care
Read this article at
Abstract
Background
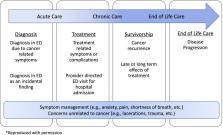
The global prevalence of cancer is rapidly increasing and will increase the acute care needs of patients with cancer, including emergency department (ED) care. Patients with cancer present to the ED across the cancer care continuum from diagnosis through treatment, survivorship, and end-of-life. This article describes the characteristics and determinants of ED visits, as well as challenges in the effort to define preventable ED visits in this population.
Findings
The most recent population-based estimates suggest 4% of all ED visits are cancer-related and roughly two thirds of these ED visits result in hospitalization—a 4-fold higher ED hospitalization rate than the general population. Approximately 44% of cancer patients visit the ED within 1 year of diagnosis, and more often have repeat ED visits within a short time frame, though there is substantial variability across cancer types. Similar patterns of cancer-related ED use are observed internationally across a range of different national payment and health system settings. ED use for patients with cancer likely reflects a complex interaction of individual and contextual factors—including provider behavior, health system characteristics, and health policies—that warrants greater attention in the literature.
Conclusions
Given the amount and complexity of cancer care delivered in the emergency setting, future research is recommended to examine specific symptoms associated with cancer-related ED visits, the contextual determinants of ED use, and definitions of preventable ED use specific to patients with cancer.
Related collections
Most cited references80
- Record: found
- Abstract: found
- Article: not found
Projections of the cost of cancer care in the United States: 2010-2020.
- Record: found
- Abstract: not found
- Article: not found