- Record: found
- Abstract: found
- Article: found
Lung cancer in the emergency department
Read this article at
Abstract
Background
Though decreasing in incidence and mortality in the USA, lung cancer remains the deadliest of all cancers. For a significant number of patients, the emergency department (ED) provides the first pivotal step in lung cancer prevention, diagnosis, and management. As screening recommendations and treatments advance, ED providers must stay up-to-date with the latest lung cancer recommendations. The purpose of this review is to identify the many ways that emergency providers may intersect with the disease spectrum of lung cancer and provide an updated array of knowledge regarding detection, management, complications, and interdisciplinary care.
Findings
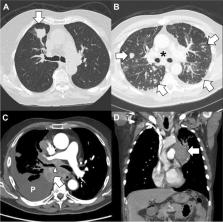
Lung cancer, encompassing 10–12% of cancer-related emergency department visits and a 66% admission rate, is the most fatal malignancy in both men and women. Most patients presenting to the ED have not seen a primary care provider or undergone screening. Ultimately, half of those with a new lung cancer diagnosis in the ED die within 1 year. Incidental findings on computed tomography are mostly benign, but emergency staff must be aware of the factors that make them high risk. Radiologic presentations range from asymptomatic nodules to diffuse metastatic lesions with predominately pulmonary symptoms, and some may present with extra-thoracic manifestations including neurologic. The short-term prognosis for ED lung cancer patients is worse than that of other malignancies. Screening offers new hope through earlier diagnosis but is underutilized which may be due to racial and socioeconomic disparities. New treatments provide optimism but lead to new complications, some long-term. Multidisciplinary care is essential, and emergency medicine is responsible for the disposition of patients to the appropriate specialists at inpatient and outpatient centers.
Conclusion
ED providers are intimately involved in all aspects of lung cancer care. Risk factor modification and referral for lung cancer screening are opportunities to further enhance patient care. In addition, with the advent of newer cancer therapies, ED providers must stay vigilant and up-to-date with all aspects of lung cancer including disparities, staging, symptoms of disease, prognosis, treatment, and therapy-related complications.
Related collections
Most cited references123
- Record: found
- Abstract: found
- Article: not found
Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries
- Record: found
- Abstract: found
- Article: not found
Cancer statistics, 2022
- Record: found
- Abstract: found
- Article: not found