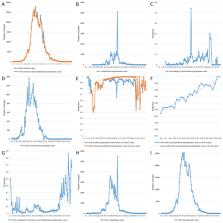
In late February, 2022, a wave of SARS-CoV-2 infection rapidly appeared in Shanghai, China. According to the Shanghai Municipal Health Commission, as of May 4, 2022, 601 942 cases have been identified, including 547 056 asymptomatic carriers. 503 people have died with or from COVID-19. Phylogenetic features of SARS-CoV-2 viral genomes from 129 patients in this period, and inferring their relationship with those available on the GISAID database, indicated that all of the new viral genomes in Shanghai were clustered into the SARS-CoV-2 BA.2.2 sub-lineage. Of note, BA.2 is a sub-lineage of the omicron variant of SARS-CoV-2 (B.1.1.159). Multiple sub-lineages of BA.2 have been characterised, many of which appear to show distinct regional distribution patterns. At present, BA2.2 only represents a small sub-lineage of BA.2 worldwide (1993 [0·25%] of 800 366 seqences in GISAID), sequences of which have been detected in Hong Kong (839 [42·10%]), the UK (742 [37·20%]), and Australia (121 [6·10%]). We assessed the potential risk of various feature mutations on BA2.2 on the severity of COVID-19 and found that these mutations showed no significance in their distributions between severe to critical and mild to moderate COVID-19, suggesting that the observed disease severity is probably mainly attributed to comorbidities. Although omicron BA.2 evolves towards less virulent, a higher rate of severe outcomes and considerable mortality have been reported in unvaccinated people, especially older adults. 1 This has been confirmed in Hong Kong, where health authorities have reported 9115 deaths among 1 192 765 people with SARS-CoV-2 (crude case fatality rate 0·76%) during the fifth wave of the pandemic, as of May 4, 2022. 2 The crude case fatality rate in those older than 60 years (19·30% of this age group has not been vaccinated) was 2·70%. Comparatively, only 2% of New Zealand's population older than 60 years has not been vaccinated, which is highly correlated with a low COVID-19 crude case fatality rate of 0·07%. In Shanghai, with a population of 25 million, the overall vaccination coverage now exceeds 90%; however, vaccination coverage has remained low in older adults—62% of 5·8 million people older than 60 years have been vaccinated, and only 38% have received a booster vaccination. As of May 4, 2022, among the 503 people who died with or from COVID-19, only 25 patients had received at least one dose of COVID-19 vaccine. The vaccination rate for the deceased patients was only 4·97%. If no strict public health measures were taken, such as large scale viral nucleic acid and antigen screening, quarantine of infected cases and close contacts in shelter hospitals and hotels, respectively, and lockdown of districts with severe outbreak, the number of severe to critical cases and the resultant death toll could be high among the older people without vaccination. The strict and comprehensive pandemic control strategies in Shanghai are therefore actually to reduce the number of people infected and to provide early diagnosis and appropriate treatment for severe COVID-19 so that the case fatality rate can be minimised, and to buy time for full vaccination coverage. Local citizens have suffered in their daily lives from inconveniences of lockdown. Some people even developed mental health symptoms as a reaction to the unexpected crisis. Facing these challenges, social workers and many volunteers have made great contributions to the care of the people in need from both material and psychological perspectives. The food and daily consumable supply are ensured thanks to the support of many other cities and provinces. Through the unprecedented efforts of health professionals in Shanghai and those coming from other cities, and of people from all the circles in Shanghai, the strategies have shown very promising results, as indicated by an R0 of 9·5 at the beginning of the wave to an Rt of 0·67 on May 1, 2022. 3 The number of newly infected cases, after peaking at 27 719 on April 13, 2022, has now dropped to 4651 cases, as of May 4, 2022. Life-saving efforts are continuing with the improvement of public health measures and social services on one hand, and treatment of hundreds of severe to critical cases on the other. Meanwhile, the return to normal life and work is proceeding in a stepwise manner, and people in Shanghai is hailing the light at the end of the tunnel. Shanghai's great efforts against omicron are essential for China to exit from the pandemic in a larger sense. As a leading economic centre and an open city in China, Shanghai has huge exchanges with other cities and regions in the country, so the spill-out of virus to other places, especially in the central and western regions with insufficient medical resources and lower vaccination coverage, could have unimaginably severe consequences. In this regard, strict control strategies in Shanghai might have prevented the continuous spread and a large number of deaths. According to the Chinese National Health Commission, 4 about 49 million people older than 60 years have not yet been vaccinated, and among this population, a considerable number suffer from underlying diseases. The persistence of dynamic zero COVID-19 community transmission in Shanghai and other cities will overcome weak links in the immunological barrier in populations across the country. Fortunately, besides the available vaccines and heterologous vaccination approach, several new vaccines specifically targeting omicron variants, including mRNA vaccine, inactivated vaccine, and recombinant Spike protein subunit vaccine, have also been approved for clinical trials in China and could soon be available for emergency use. The next challenge will be to enhance the communication between the health-care providers and the public to overcome the vaccine hesitancy and make the vaccination service accessible to all people, the older and vulnerable people in particular. Moreover, the production of effective anti-SARS-CoV-2 drugs and preparation of sufficient medical resources, including intensive care units and teams for severe diseases and training of grassroots-level health-care workers capable of last-mile services of disease control and prevention are on the way. We believe that China will win the fight against the COVID-19 pandemic in joint efforts with other members of the international community in the not too distant future. For New Zealand's COVID-19 data and statistics see https://www.health.govt.nz/covid-19-novel-coronavirus/covid-19-data-and-statistics For the Shanghai Municipal Health Commission's SARS-CoV-2 data see https://wsjkw.sh.gov.cn/