- Record: found
- Abstract: found
- Article: found
Recent Insights into the Management of Pleural Infection
Read this article at
Abstract
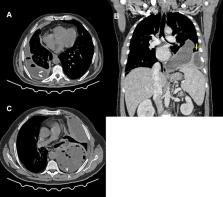
Pleural infection in adults has considerable morbidity and continues to be a life-threatening condition. The term “pleural infection” encompasses complicated parapneumonic effusions and primary pleural infections, and includes but is not limited to empyema, which refers to collection of pus in the pleural cavity. The incidence of pleural infection in adults has been continuously increasing over the past two decades, particularly in older adults, and most of such patients have comorbidities. Management of pleural infection requires prolonged duration of hospitalization (average 14 days). There are recognized differences in microbial etiology of pleural infection depending on whether the infection was acquired in the community or in a health-care setting. Anaerobic bacteria are acknowledged as a major cause of pleural infection, and thus anaerobic coverage in antibiotic regimens for pleural infection is mandatory. The key components of managing pleural infection are appropriate antimicrobial therapy and chest-tube drainage. In patients who fail medical therapy by manifesting persistent sepsis despite standard measures, surgical intervention to clear the infected space or intrapleural fibrinolytic therapy (in poor surgical candidates) are recommended. Recent studies have explored the role of early intrapleural fibrinolytics or first-line surgery, but due to considerable costs of such interventions and the lack of convincing evidence of improved outcomes with early use, early intervention cannot be recommended, and further evidence is awaited from ongoing studies. Other areas of research include the role of routine molecular testing of infected pleural fluid in improving the rate of identification of causative organisms. Other research topics include the benefit of such interventions as medical thoracoscopy, high-volume pleural irrigation with saline/antiseptic solution, and repeated thoracentesis (as opposed to chest-tube drainage) in reducing morbidity and improving outcomes of pleural infection. This review summarizes current knowledge and practice in managing pleural infection and future research directions.
Related collections
Most cited references111
- Record: found
- Abstract: found
- Article: found
Comprehensive Molecular Testing for Respiratory Pathogens in Community-Acquired Pneumonia
- Record: found
- Abstract: not found
- Article: not found
Management of pleural infection in adults: British Thoracic Society Pleural Disease Guideline 2010.
- Record: found
- Abstract: found
- Article: not found
U.K. Controlled trial of intrapleural streptokinase for pleural infection.
Author and article information
Comments
Comment on this article
 Smart Citations
Smart CitationsSee how this article has been cited at scite.ai
scite shows how a scientific paper has been cited by providing the context of the citation, a classification describing whether it supports, mentions, or contrasts the cited claim, and a label indicating in which section the citation was made.