- Record: found
- Abstract: found
- Article: found
Globally prevalent PfMDR1 mutations modulate Plasmodium falciparum susceptibility to artemisinin-based combination therapies

Read this article at
Abstract
Antimalarial chemotherapy, globally reliant on artemisinin-based combination therapies (ACTs), is threatened by the spread of drug resistance in Plasmodium falciparum parasites. Here we use zinc-finger nucleases to genetically modify the multidrug resistance-1 transporter PfMDR1 at amino acids 86 and 184, and demonstrate that the widely prevalent N86Y mutation augments resistance to the ACT partner drug amodiaquine and the former first-line agent chloroquine. In contrast, N86Y increases parasite susceptibility to the partner drugs lumefantrine and mefloquine, and the active artemisinin metabolite dihydroartemisinin. The PfMDR1 N86 plus Y184F isoform moderately reduces piperaquine potency in strains expressing an Asian/African variant of the chloroquine resistance transporter PfCRT. Mutations in both digestive vacuole-resident transporters are thought to differentially regulate ACT drug interactions with host haem, a product of parasite-mediated haemoglobin degradation. Global mapping of these mutations illustrates where the different ACTs could be selectively deployed to optimize treatment based on regional differences in PfMDR1 haplotypes.
Abstract
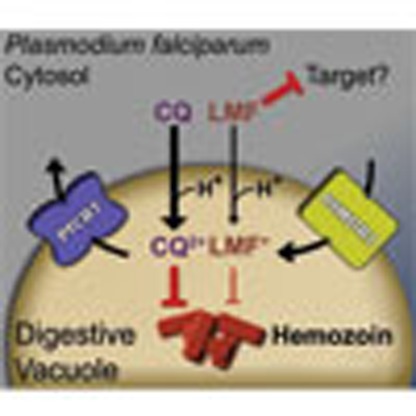 Antimalarial chemotherapy relies on combination therapies (ACTs) consisting of an
artemisinin derivative and a partner drug. Here, the authors study the effects of
globally prevalent mutations in a multidrug resistance transporter (PfMDR1) on the
parasite's susceptibility to ACT drugs.
Antimalarial chemotherapy relies on combination therapies (ACTs) consisting of an
artemisinin derivative and a partner drug. Here, the authors study the effects of
globally prevalent mutations in a multidrug resistance transporter (PfMDR1) on the
parasite's susceptibility to ACT drugs.
Related collections
Most cited references51
- Record: found
- Abstract: found
- Article: not found
Mefloquine resistance in Plasmodium falciparum and increased pfmdr1 gene copy number.
- Record: found
- Abstract: found
- Article: not found
Dihydroartemisinin-piperaquine resistance in Plasmodium falciparum malaria in Cambodia: a multisite prospective cohort study.
- Record: found
- Abstract: found
- Article: not found