- Record: found
- Abstract: found
- Article: found
Encuesta sobre la actividad de los laboratorios de función pulmonar. Efectos durante la pandemia por SARS-CoV-2 Translated title: National Survey on the Activity of Lung Function Laboratories. Effects During the SARS-COV-2 Pandemic
Read this article at
Abstract
Introducción
A raíz de la pandemia de SARS-CoV-2 en marzo del 2020 los laboratorios de función pulmonar (LFP) sufrieron una transformación, con la reducción del número de pruebas o cierre en algunos casos. El objetivo de este trabajo fue conocer la actividad de los LFP en España y la modificación de esta debido a la pandemia.
Material y métodos
Se realizó una encuesta protocolizada a los miembros de los LFP a través de la Sociedad Española de Neumología y Cirugía Torácica (SEPAR).
Resultados
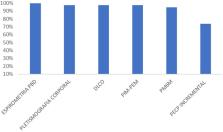
Contestaron 39 hospitales del territorio nacional. Las pruebas de función pulmonar que más se realizaban en los LFP fueron: espirometría forzada con prueba broncodilatadora (100%), pletismografía corporal (97,4%), capacidad de transferencia CO (97,4%), fuerza de los músculos respiratorios medidos en boca (97,4%), prueba de la marcha de 6 min (94,7%), medición de fracción exhalada de óxido nítrico (92,3%) y prueba de esfuerzo incremental (71,8%).
La pandemia produjo un descenso significativo en el número de pruebas (35,4%) durante el 2020 con posterior recuperación en el 2021, sin llegar a valores prepandemia.
Los cambios más importantes fueron: incremento en los tiempos de exploración, el trabajo con equipos de protección individual y la ventilación de los espacios. La realización del frotis nasofaríngeo para estudio de SARS-CoV-2 previo a las pruebas no fue homogénea en los LFP.
Translated abstract
Following the SARS-CoV-2 pandemic in March 2020, pulmonary function testing (PFT) laboratories underwent a transformation, with a reduction in the number of tests or closure in some cases. The aim of this work was to know the activity of PFT in Spain and the modification of this activity due to the pandemic.
A protocolised survey was carried out to members of the PFT laboratories through the Spanish Society of Pneumology and Thoracic Surgery (SEPAR).
Thirty-nine hospitals in Spain responded. The pulmonary function tests most frequently performed in the PFT laboratories were forced spirometry with bronchodilator test (100%), body plethysmography (97.4%), CO transfer capacity (97.4%), respiratory muscle strength measured in the mouth (97.4%), 6-minute walking test (94.7%), measurement of exhaled fraction of nitric oxide (92.3%) and incremental exercise test (71.8%).
The pandemic led to a significant decrease in the number of tests (35.4%) during 2020 with subsequent recovery in 2021, without reaching pre-pandemic values.
The most important changes were increased examination times, working with personal protective equipment and ventilation of the rooms. The performance of the nasopharyngeal swab for SARS-CoV2 testing prior to the tests was not homogeneous in the PFT laboratories.
Related collections
Most cited references9
- Record: found
- Abstract: found
- Article: not found
Multi-ethnic reference values for spirometry for the 3-95-yr age range: the global lung function 2012 equations.
- Record: found
- Abstract: found
- Article: not found
Respiratory function in patients post-infection by COVID-19: a systematic review and meta-analysis
- Record: found
- Abstract: found
- Article: not found