- Record: found
- Abstract: found
- Article: found
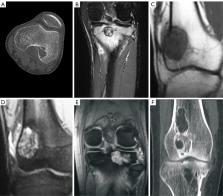
Images of giant cell tumor and chondroblastoma around the knee: retrospective analysis of 99 cases
Read this article at
Abstract
Background
It is difficult to differentiate giant cell tumors of the bone (GCTB) from chondroblastoma around the knee based on imaging findings. This study analyzed the imaging features of these 2 diseases for better differentiation.
Methods
This retrospective cross-sectional cohort study reviewed data of patients with pathologically confirmed GCTB (n=81; age 15–75 years; median age 33 years) and chondroblastoma (n=18; age 12–34 years; median age 14 years). In all, 18 imaging signs were analyzed.
Results
Patients with chondroblastoma were relatively younger than those with GCTB. On imaging, lesion length was significantly (P<0.00001) smaller in chondroblastoma [range, 15.80–78.30 mm; mean ± standard deviation (SD) 34.15±18.24 mm; 95% confidence interval (CI): 24.05–44.25 mm] than in GCTB [range, 30.10–117.50 mm; mean ± SD 59.73±15.28 mm; 95% CI: 56.24–63.22 mm]. Significantly more (P<0.05) chondroblastoma lesions had calcification (76.5% vs. 1.3%), lobulation (77.8% vs. 32.1%), and swelling range >15 mm (84.6% vs. 41.1%) than did GCTB lesions, whereas significantly more (P<0.05) GCTB lesions were greater than half the host bone diameter (74.1% vs. 16.7%) and had a lesion long axis that was consistent with that of the host bone (98.8% vs. 27.8%). There were no significant differences (P>0.05) between the 2 tumors in the remaining 11 imaging signs.
Conclusions
A narrow zone of transition, intratumor calcification, lobulation, tumor transverse diameter greater than the bone diameter, maximum lesion length, consistency between the tumor and bone long axes, and edema range around the lesion >15 mm are parameters that can be used to differentiate GCTB from chondroblastoma around the knee.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
Giant cell tumor of bone: review, mimics, and new developments in treatment.
- Record: found
- Abstract: found
- Article: not found
From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: radiologic-pathologic correlation.
- Record: found
- Abstract: found
- Article: not found