- Record: found
- Abstract: found
- Article: found
Perspectives of Young Adults on Receiving Telepsychiatry Services in an Urban Early Intervention Program for First-Episode Psychosis: A Cross-Sectional, Descriptive Survey Study
Read this article at
Abstract
Background
Limited knowledge exists on telepsychiatry in specialized services for first-episode psychosis (FEP), despite its potential for improving service access and engagement.
Objective
To explore access and use of technology, obstacles to attending clinic appointments, and perspectives of young adults with FEP on using telepsychiatry as part of outpatient services.
Methods
A cross-sectional, descriptive survey study was conducted between July and October 2017 with young adults between the ages of 18 and 38 recruited from a specialized program for FEP in an urban Canadian setting. Data were analysed using descriptive statistics and content analysis.
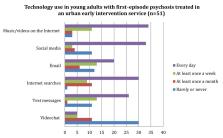
Results
Among 51 participants (mean age = 26.1, SD = 4.2; 59% male; 20% experiencing housing instability), more than half (59%, n = 30) rarely or never used mainstream video chat (e.g., Facetime). The majority (78%, n = 40) reported obstacles to attending appointments, with several (37%, n = 19) identifying two or more. Almost half (49%, n = 25) were very favorable towards telepsychiatry and a quarter (25%, n = 13) were somewhat favorable. Participants expressed several concerns about telepsychiatry, including loss of human contact and confidentiality.
Conclusions
To our knowledge, this is a first study on the perspectives of individuals with FEP about telepsychiatry. Despite experiencing obstacles to attending appointments and expressing receptivity towards telepsychiatry, participants did not have access to these services. It is important to provide education to clinicians on the potential of telepsychiatry to improve service access. Also, more research is needed on when, where, and how telepsychiatry can be integrated into existing care while addressing patient and clinician concerns.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
A systematic review of patient acceptance of consumer health information technology.
- Record: found
- Abstract: found
- Article: not found
Telepsychiatry: videoconferencing in the delivery of psychiatric care.
- Record: found
- Abstract: found
- Article: not found