- Record: found
- Abstract: found
- Article: found
Right ventricular mechanical pattern in health and disease: beyond longitudinal shortening
Read this article at
Abstract
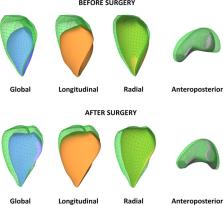
Right ventricular (RV) function has proven to be a prognostic factor in heart failure with reduced and preserved ejection fraction and in pulmonary hypertension. RV function is also a cornerstone in the management of novel clinical issues, such as mechanical circulatory support devices or grown-up congenital heart disease patients. Despite the notable amount of circumferentially oriented myofibers in the subepicardial layer of the RV myocardium, the non-longitudinal motion directions are often neglected in the everyday assessment of RV function by echocardiography. However, the complex RV contraction pattern incorporates different motion components along three anatomically relevant axes: longitudinal shortening with traction of the tricuspid annulus towards the apex, radial motion of free wall often referred as the “bellows effect”, and anteroposterior shortening of the chamber by stretching the free wall over the septum. Advanced echocardiographic techniques, such as speckle-tracking and 3D echocardiography allow an in-depth characterization of RV mechanical pattern, providing better understanding of RV systolic and diastolic function. In our current review, we summarize the existing knowledge regarding RV mechanical adaptation to pressure- and/or volume-overloaded states and also other physiologic or pathologic conditions.
Related collections
Most cited references43

- Record: found
- Abstract: found
- Article: found
Repaired tetralogy of Fallot: the roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support
- Record: found
- Abstract: found
- Article: not found