- Record: found
- Abstract: found
- Article: found
Measles-Rubella Supplementary Immunization Activity Readiness Assessment — India, 2017–2018
research-article
Vandana Gurnani , MA
1 ,
Pradeep Haldar , MD
1 ,
Sudhir Khanal , MBBS
2
,
,
Pankaj Bhatnagar , MD
3 ,
Balwinder Singh , MBBS
3 ,
Danish Ahmed , MBBS
3 ,
Mohammad Samiuddin , MBBS
3 ,
Arun Kumar , MSc
3 ,
Yashika Negi , MD
1 ,
Satish Gupta , MD
4 ,
Pauline Harvey , PhD
3 ,
Sunil Bahl , MD
2 ,
Alya Dabbagh , PhD
5 ,
James P. Alexander , MD
6 ,
James L. Goodson , MPH
6
06 July 2018
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
In 2013, during the 66th session of the Regional Committee of the World Health Organization
(WHO) South-East Asia Region (SEAR), the 11 SEAR countries* adopted goals to eliminate
measles and control rubella and congenital rubella syndrome by 2020
†
(
1
). To accelerate progress in India (
2
,
3
), a phased
§
nationwide supplementary immunization activity (SIA)
¶
using measles-rubella vaccine and targeting approximately 410 million children aged
9 months–14 years commenced in 2017 and will be completed by first quarter of 2019.
To ensure a high-quality SIA, planning and preparation were monitored using a readiness
assessment tool adapted from the WHO global field guide** (
4
) by the India Ministry of Health and Family Welfare. This report describes the results
and experience gained from conducting SIA readiness assessments in 24 districts of
three Indian states (Andhra Pradesh, Kerala, and Telangana) during the second phase
of the SIA. In each selected area, assessments were conducted 4–6 weeks and 1–2 weeks
before the scheduled SIA. At the first assessment, none of the states and districts
were on track with preparations for the SIA. However, at the second assessment, two
(67%) states and 21 (88%) districts were on track. The SIA readiness assessment identified
several preparedness gaps; early assessment results were immediately communicated
to authorities and led to necessary corrective actions to ensure high-quality SIA
implementation.
Supplemental Immunization Activity Readiness Assessment Process
SIA readiness assessments were conducted in 24 (41%) of the 58 districts in the states
of Andhra Pradesh (seven districts), Kerala (five), and Telangana (12). In addition,
74 (72%) of 103 blocks
††
in Telangana were selected for readiness assessments. Districts and blocks were selected
for assessment based on low routine vaccination coverage, difficult-to-reach populations,
high proportion of urban to rural population, and categorization as polio high-risk
based on polio risk assessments.
The assessments were conducted by teams coordinated by the WHO India Country Office.
The teams included members from the India Ministry of Health and Family Welfare, especially
the Immunization Technical Support Unit, National Institute of Health and Family Welfare,
and senior immunization program officers from other states; United Nations agencies,
including WHO, United Nations Children's Fund (UNICEF), and United Nations Development
Program; and nongovernmental organizations, including John Snow Inc., Global Health
Strategies, CORE Group Polio Project, and others.
The India SIA readiness assessment tool and checklists were adapted from the WHO field
guide for planning and implementing SIAs (
4
) according to the India national measles-rubella SIA operational guidelines, for
use at the national, state, district, and block levels. Assessment teams reviewed
preparations in planning and coordination, advocacy, accountability, management of
adverse events following immunization, vaccines and logistics management, funding,
and communication, using checklists modified at each level based on expected functions
of SIA components for that level (Table 1). The checklists included questions with
possible answers of “yes” or “no.” The overall percentage of affirmative responses
was calculated, and the assessed area was categorized as “on track” (≥80%), “needs
work” (60%–79%), or “not ready” (<60%).
TABLE 1
Questions on supplementary immunization activities readiness assessment checklist,
by component — India, 2017–2018
Component
Activity
Planning and coordination
State/District SIA Steering Committee met at least once?
Did all essential government officials participate in at least one State Task Force
for Immunization (STFI) meeting?*
Circle those who did not participate: Permanent Secretary/State Education Officer/State
Program Officer/Women and Child Development/Integrated Child Development Services/Minority
Welfare Officer*
Did essential non-governmental stakeholders participate in at least one STFI meeting?*
Circle those who did not participate: Indian Medical Association (IMA)/Indian Academy
of Pediatrics (IAP)/private practitioners/LIONS International/religious leaders.*
State/district Immunization Officer or other state level monitors using state checklist-A
for tracking progress of state level preparedness?
State/district Immunization Officer using checklist-B for tracking progress by visiting
the priority districts?*
State/district monitors identified for visiting the priority districts for assessing
the SIA preparedness?
State/district Education Officer communicated with all District Education Officer?
State/district Program Officer communicated with all Child Development Project Officers?
Has the state committee for adverse events following immunization (AEFI) met at least
once?
Sensitization meetings
Sensitization meeting held with heads of IMA and IAP, including leading private practitioners?*
Sensitization meeting held with district level Education Officers?
Coordination meeting with state level representatives of public schools, private schools’
associations, religious institutions, etc.?*
Vaccine logistics and management
Adequate quantity of vaccine and diluents available per microplan? (consider planned
staggered distribution of vaccine)
Adequate quantity of auto-disable syringes and mixing syringes available per microplan?
(consider planned staggered distribution of vaccine)
Adequate quantity of indelible marker pens available per microplan? Vaccine distribution
plan available for districts?
Funds
Has state received funds from the national level?
Has state disseminated financial guidelines to all districts?
Communication planning
Is there a nodal officer, other than State EPI Officer, designated for SIA communication
planning at state level?
At least one joint meeting held for secretaries of Health, Education, other department?
(check for official circular)
State communication core group formed and held at least one meeting? (verify meeting
minutes)*
SIA communication plan prepared in a template as per operational guidelines?
All districts/blocks have submitted communication plan in prescribed template?
Received guidelines for communication activities including financial for SIA and shared
with all districts? (check for official circular)*
State/district implementing communication plan for underserved communities? (identified
influencers, religious and educational institutions for support)*
Was there discussion on communication planning in STFI? (verify meeting minutes)
Communication and social mobilization
Printed and distributed all IEC (Information, Education, and Communication) materials
or guidelines?
Identified local celebrities or champion for SIA? (verify how involved in SIA)
State/district launch or inauguration for SIA? (confirm date for launch)
Advocacy
Sensitization meeting with religious leaders or influencers planned/held?
Media and social media
State/district has identified media spokesperson for the SIA?
Media workshop planned at state level for SIA? (confirm dates for media workshop)
Is an official or agency regularly tracking media and social media for SIA and immunization
messages? (collect related news articles)*
Task force for social media was formed? (confirm at least one responsible person designated
at state level for managing social media)
WhatsApp group(s) was formed for health, education, and immunization-related sectors?
Facebook page was created for the SIA? (check the page for SIA post)*
* These variables were considered to be critical and were evaluated subjectively by
the assessment team to decide "go" or "delayed go" for an area marked as "needs work."
The checklists used at state, district, planning unit, and school levels were modified
to reflect the level-specific role and function for each component.
The first readiness assessment was conducted 4–6 weeks before the SIA and the second,
1–2 weeks before the SIA. A decision either to start the SIA on the designated date
or to delay the SIA until preparations were complete was made at the district and
state levels, based on the second assessment score and categorization of the district
or state assessed. Those areas categorized as on track were permitted to start the
SIA (“go”); those categorized as not ready were delayed (“delayed go”); and those
categorized as needing work either started or delayed the SIA, based on subjective
evaluation by the assessment team of critical gaps and level of commitment to taking
corrective actions in a timely manner. At the end of the assessment, evidence-based
feedback from the teams was shared with health and administration leaders at district,
state, and national levels to facilitate decision-making for strengthening the quality
of this and future SIAs.
Supplemental Immunization Activity Readiness Assessment Results
At the first assessment, none of the three states and none of the 24 districts was
on track (Table 2). The challenges most frequently identified during the preparedness
assessment were lack of logistics and training materials and nonengagement of schools.
Based on feedback provided, state-level program managers initiated corrective actions
in all districts. At the second assessment, Kerala and Telangana states were on track;
Andhra Pradesh needed work and had to delay the start of the SIA to provide an additional
week for preparation. Overall, 19 (79%) of the 24 districts were on track (including
information, education, and communication [IEC] readiness), four (17%) needed additional
work and undertook minor corrective actions, and one (4%) was not ready and had a
delayed go.
TABLE 2
Supplementary immunization activity readiness assessment* results — three states,
India, 2017–2018
SIA readiness assessment results
State (no. of districts)
Andhra Pradesh (7)
Kerala (5)
Telangana (12)
First assessment
Not ready, no. (%)
5 (71)
1 (20)
10 (83)
Needs work, no. (%)
2 (29)
4 (80)
2 (17)
On track, no. (%)
0 (0)
0 (0)
0 (0)
Key findings
State level trainings not started
No SIA logistics plan available
IEC materials not available
IEC materials not available
No schools aware of SIA
No clarity on SIA financial guidelines
Most schools not informed
Trainings conducted without training materials
Private schools not on board
Medical fraternity not involved and informed about SIA
High level of vaccine hesitancy and frank refusal in one district
Informal educational institutions, religious schools, madrasas not in target population
Low level SIA awareness
No clarity on financial guidelines for local implementers
Low level preparedness for management of AEFI
Language barriers
Lack of SIA awareness
Vaccine hesitancy in minority communities
Actions taken
Video conference with all districts by the principal secretary and by each district
to all blocks to discuss assessment findings and plan corrective actions
SIA logistics made immediately available to the districts
Video conference with all deputy commissioners, chief medical officers, and district
immunization officers requesting immediate corrective actions
Principal secretary visited all high-risk districts to get firsthand information on
preparedness progress and next steps
Microplans reviewed in all areas; additional field monitors deployed in high-risk
districts and blocks
Meeting with district education officers to develop plan; directives for noncompliant
schools, meeting with heads of madrasas organized to encourage SIA participation
Operational communication plan developed with all partners; all district microplans
reviewed
Additional communication and social mobilization officers mobilized in areas with
vaccine hesitancy and refusal
Prominent talk show personalities appear on local television channels; media release
in Urdu language; video of prominent opinion leaders and religious leaders developed
and circulated through social media platform
Medical and Indian Academy of Pediatrics invited to participate in process and promote
SIA in local newspaper
Medical colleges and medical fraternity brought on board as support group to the SIA
District magistrates briefed on assessment results; called all immunization offices
and received regular updates on progress to accelerate preparedness
Senior state officers visited high-risk areas to accelerate preparedness activities
District AEFI committee reactivated and capacity building done
Administrative processes to print and deploy materials were fast-tracked. Orientation
on financial guidelines
Meeting with district governors of Lions Clubs International and request to adopt
problematic schools to accelerate SIA preparedness and awareness
Second assessment
Not ready, no. (%)
1 (14)
0 (0)
0 (0)
Needs work, no. (%)
3 (43)
0 (0)
1 (8)
On track, no. (%)
3 (43)
5 (100)
11 (92)
Decision
Delay
Move forward
Move forward
% Administrative coverage, state (districts range)
97 (86 to >100)
89 (87 to 98)
>100 (87 to >100)
Abbreviations: AEFI = adverse events following immunization; IEC = information, education,
and communication; SIA = supplementary immunization activity.
* SIA readiness assessments during planning for phase 2 of the nationwide SIA using
measles-rubella vaccine for children aged 9 months–14 years that started in 2017.
The first readiness assessment was conducted at 4–6 weeks before the SIA and the second
assessment at 1–2 weeks before the SIA. Checklists had questions with possible answers
of “Yes” or “No.” Scoring was based on percentage of “Yes” responses, categorized
as on track (≥80%), needs work (60%–79%), and not ready (<60%). Administrative coverage
>100% indicated the intervention reached more persons than were in the estimated target
population.
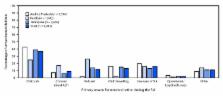
During the SIA, rapid convenience monitoring, a programmatic tool that identifies
children not vaccinated during the campaign and compiles reasons for nonvaccination,
determined that 9,912 (6.9%) of all 143,894 targeted children were not vaccinated
during the SIA, including 7% (3,314 of 44,906) in Andhra Pradesh, 10% (1,943 of 19,408)
in Kerala, and 6% (4,659 of 79,580) in Telangana (Figure). Among all unvaccinated
children located through rapid convenience monitoring, the most frequently reported
reason given by caregivers for not vaccinating was that the child was sick (3,715;
37%), followed by lack of awareness of the campaign (1,566; 16%). In Kerala, refusal
accounted for approximately a quarter of children who were not vaccinated. The least
frequently reported reason (209; 2%) for nonvaccination was SIA operational gaps (e.g.,
nonfunctioning vaccination sites, absent or late vaccinators, vaccine stock-outs,
and other logistics issues) (Figure). Reported SIA administrative coverage was ≥95%
in two states and 17 districts (Table 2).
FIGURE
Percentage of unvaccinated children, by reported primary reason for nonvaccination*
during supplementary immunization activity
†
(phase 2)
§
— Andhra Pradesh, Kerala, and Telangana states, India, 2017–2018
Abbreviations: AEFI = Adverse events following immunization; MR = measles-rubella;
SIA = supplementary immunization activity.
* Intra-SIA monitoring using rapid convenience monitoring.
† Nationwide SIA using MR vaccine for children aged 9 months–14 years.
§ Phase 2 of phased nationwide SIA started in 2017 and to be completed by first quarter
of 2019. Children targeted for vaccination during phase 2 of the SIA but not vaccinated
included 7% in Andhra Pradesh, 10% in Kerala, and 6% in Telangana.
The figure above is a bar chart showing the percentage of unvaccinated children, by
reported primary reason for nonvaccination, during phase 2 of a supplementary immunization
activity in the states of Andhra Pradesh, Kerala, and Telangana in India during 2017–2018.
Discussion
Experience with the SIA assessment in India demonstrated that the WHO SIA readiness
assessment tool and procedures were useful for ensuring preparedness for implementation
of a high-quality SIA. Corrective actions implemented after the first assessment,
which found that two thirds of districts were not ready for the SIA, resulted in 79%
of districts being on track by the second assessment. Providing feedback to key decision-makers
immediately after the assessments helped with planning and allocation of resources
and facilitated implementation of timely corrections. These midcourse corrections
also might have resulted in further-reaching effects across each of the three states
because of the statewide directives issued by immunization program managers for corrective
actions in all districts to better prepare for this SIA and future SIAs.
As suggested in the global guidelines, decision-makers in India used the terminology
“delayed go” rather than “no go” in states and districts assessed as not ready for
the measles-rubella SIA, to provide positive reinforcement to immunization program
personnel who needed additional time for preparation. Intra-SIA rapid convenience
monitoring found that SIA operational gaps were the least common reason for children
not being vaccinated, an indication of good preparation and implementation of campaign
activities. The primary reasons for children not being vaccinated during the SIA were
related to IEC gaps and challenges in addressing parental misperceptions and their
lack of awareness of and availability for the SIA. These findings suggest that the
WHO SIA readiness checklists section on IEC and communication strategies might need
to be revised and expanded.
Although WHO global guidance recommends four to six assessments before an SIA to ensure
readiness, in this setting, only two pre-SIA assessments were designed and conducted
in each area. Because the SIA readiness assessment process was part of the overall
operational activities and covered by the existing technical assistance of WHO, UNICEF,
and partners, no additional costs were budgeted for the activity. However, inclusion
of more districts, blocks, and health centers in the process could help to ensure
homogeneous quality of SIA implementation.
The findings in this report are subject to at least two limitations. First, the selection
of areas for readiness assessments included in this report was purposeful, and no
control groups were available for comparison. Second, the impact of the readiness
assessments on achieving the ≥95% SIA coverage target was not assessed by post-SIA
surveys because of time and resource limitations and lack of a comparison group.
The WHO South-East Asia Region aims to vaccinate >500 million children with measles-rubella
vaccine through SIAs by 2019. The experience with pre-SIA assessments in India reported
here will help improve preparedness for high-quality SIAs, ensuring high vaccination
coverage to achieve the regional goal of measles elimination and rubella and congenital
rubella syndrome control by 2020.
Summary
What is already known about this topic?
India has adopted a goal for measles elimination and rubella and congenital rubella
syndrome control by 2020 by achieving high coverage with 2 routine doses of measles-containing
vaccine and supplemental immunization activities (SIAs), which require substantial
preparation.
What is added by this report?
Two pre-SIA readiness assessments in 24 districts in three states provided feedback
to decision-makers that led to corrective actions. Readiness improved from 33% to
79% between the two assessments.
What are the implications for public health practice?
The WHO South-East Asia Region aims to vaccinate >500 million children with measles-rubella
vaccine through SIAs by 2019. The experience with pre-SIA assessments can help improve
preparedness and ensure high coverage through SIAs in the region.
Related collections
Most cited references1
- Record: found
- Abstract: found
- Article: found
Progress Toward Regional Measles Elimination — Worldwide, 2000–2016
Alya Dabbagh, Minal K Patel, Laure Dumolard … (2017)