- Record: found
- Abstract: found
- Article: found
Shining the Spotlight on Multiple Daily Insulin Therapy: Real-World Evidence of the InPen Smart Insulin Pen
Read this article at
Abstract
Objective:
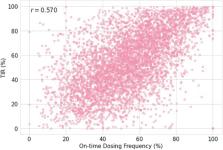
Connected insulin pens are creating opportunities for the millions of individuals with diabetes using multiple daily injections (MDI) therapy across the globe. Continuous glucose monitoring (CGM) data from connected insulin pens are revealing gaps and opportunities to significantly improve care for this population. In this article, we report real-world findings of the InPen™ smart insulin pen paired with CGM (InPen system), used by persons with type 1 diabetes (T1D) and type 2 diabetes (T2D).
Methods:
A retrospective cohort analysis was conducted with the real-world data collected from the InPen system of individuals ( N = 3793 with T1D, N = 552 with T2D, and N = 808 unidentified) who used the system from January 01, 2020, to December 31, 2021. Diabetes management (e.g., missed and mistimed insulin dosing, mismatched food intake, and correction dose delivery) and glycemic outcomes were assessed.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
State of Type 1 Diabetes Management and Outcomes from the T1D Exchange in 2016–2018
- Record: found
- Abstract: found
- Article: not found