- Record: found
- Abstract: found
- Article: found
Acute reperfusion therapies for acute ischemic stroke patients with unknown time of symptom onset or in extended time windows: an individualized approach
Read this article at
Abstract
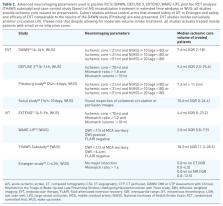
Recent randomized controlled clinical trials (RCTs) have revolutionized acute ischemic stroke care by extending the use of intravenous thrombolysis and endovascular reperfusion therapies in time windows that have been originally considered futile or even unsafe. Both systemic and endovascular reperfusion therapies have been shown to improve outcome in patients with wake-up strokes or symptom onset beyond 4.5 h for intravenous thrombolysis and beyond 6 h for endovascular treatment; however, they require advanced neuroimaging to select stroke patients safely. Experts have proposed simpler imaging algorithms but high-quality data on safety and efficacy are currently missing. RCTs used diverse imaging and clinical inclusion criteria for patient selection during the dawn of this novel stroke treatment paradigm. After taking into consideration the dismal prognosis of nonrecanalized ischemic stroke patients and the substantial clinical benefit of reperfusion therapies in selected late presenters, we propose rescue reperfusion therapies for acute ischemic stroke patients not fulfilling all clinical and imaging inclusion criteria as an option in a subgroup of patients with clinical and radiological profiles suggesting low risk for complications, notably hemorrhagic transformation as well as local or remote parenchymal hemorrhage. Incorporating new data to treatment algorithms may seem perplexing to stroke physicians, since treatment and imaging capabilities of each stroke center may dictate diverse treatment pathways. This narrative review will summarize current data that will assist clinicians in the selection of those late presenters that will most likely benefit from acute reperfusion therapies. Different treatment algorithms are provided according to available neuroimaging and endovascular treatment capabilities.
Related collections
Most cited references181
- Record: found
- Abstract: not found
- Article: not found
2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation
- Record: found
- Abstract: found
- Article: not found
Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association
- Record: found
- Abstract: found
- Article: not found