- Record: found
- Abstract: found
- Article: found
Head-neck movement may predispose to the development of arytenoid dislocation in the intubated patient: a 5-year retrospective single-center study
Read this article at
Abstract
Background
Arytenoid dislocation is a rare laryngeal injury that may follow endotracheal intubation. We aimed to determine the incidence and risk factors for arytenoid dislocation after surgery under general anaesthesia.
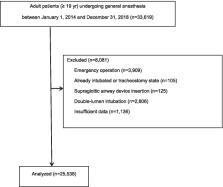
Methods
We reviewed the medical records of patients who underwent operation under general anaesthesia with endotracheal intubation from January 2014 to December 2018. Patients were divided into the non-dislocation and dislocation groups depending on the presence or absence of arytenoid dislocation. Patient, anaesthetic, and surgical factors associated with arytenoid dislocation were determined using Poisson regression analysis.
Results
Among the 25,538 patients enrolled, 33 (0.13%) had arytenoid dislocation, with higher incidence after anterior neck and brain surgery. Patients in the dislocation group were younger (52.6 ± 14.4 vs 58.2 ± 14.2 yrs, P = 0.025), more likely to be female (78.8 vs 56.5%, P = 0.014), and more likely to be intubated by a first-year anaesthesia resident (33.3 vs 18.5%, P = 0.048) compared to those in the non-dislocation group. Patient positions during surgery were significantly different between the groups ( P = 0.000). Multivariable Poisson regression identified head-neck positioning (incidence rate ratio [IRR], 3.10; 95% confidence interval [CI], 1.50–6.25, P = 0.002), endotracheal intubation by a first-year anaesthesia resident (IRR, 2.30; 95% CI, 1.07–4.64, P = 0.024), and female (IRR, 3.05; 95% CI, 1.38–7.73, P = 0.010) as risk factors for arytenoid dislocation.
Conclusion
This study showed that the incidence of arytenoid dislocation was 0.13%, and that head-neck positioning during surgery, less anaesthetist experience, and female were significantly associated with arytenoid dislocation in patients who underwent surgeries under general anaesthesia with endotracheal intubation.
Related collections
Most cited references34
- Record: found
- Abstract: found
- Article: not found
Postoperative throat complaints after tracheal intubation.
- Record: found
- Abstract: not found
- Article: not found
Postoperative sore throat after ambulatory surgery
- Record: found
- Abstract: found
- Article: not found