- Record: found
- Abstract: found
- Article: found
Changing the System - Major Trauma Patients and Their Outcomes in the NHS (England) 2008–17
Read this article at
Abstract
Background
Trauma care in England was re-organised in 2012 with ambulance bypass of local hospitals to newly designated Major Trauma Centres (MTCs). There is still controversy about the optimal way to organise health series for patients suffering severe injury.
Methods
A longitudinal series of annual cross-sectional studies of care process and outcomes from April 2008 to March 2017. Data was collected through the national clinical audit of major trauma care. The primary analysis was carried out on the 110,863 patients admitted to 35 hospitals that were ‘consistent submitters’ throughout the study period. The main outcome was longitudinal analysis of risk adjusted survival.
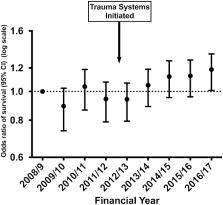
Findings
Major Trauma networks were associated with significant changes in (1) patient flow (with increased numbers treated in Major Trauma Centres), (2) treatment systems (more consultant led care and more rapid imaging), (3) patient factors (an increase in older trauma), and (4) clinical care (new massive transfusion policies and use of tranexamic acid). There were 10,247 (9.2%) deaths in the 110,863 patients with an ISS of 9 or more. There were no changes in unadjusted mortality. The analysis of trends in risk adjusted survival for study hospitals shows a 19% (95% CI 3%–36%) increase in the case mix adjusted odds of survival from severe injury over the 9-year study period. Interrupted time series analysis showed a significant positive change in the slope after the intervention time point of April 2012 (+ 0.08% excess survivors per quarter, p = 0.023), in other words an increase of 0.08 more survivors per 100 patients every quarter.
Related collections
Most cited references18

- Record: found
- Abstract: found
- Article: found
Interrupted time series regression for the evaluation of public health interventions: a tutorial
- Record: found
- Abstract: found
- Article: not found
Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial.
- Record: found
- Abstract: found
- Article: not found