- Record: found
- Abstract: found
- Article: not found
Inflammatory Cytokines and Chemokines as Therapeutic Targets in Heart Failure
Read this article at
Abstract
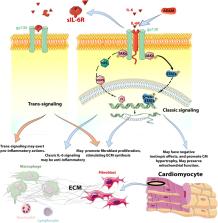
Heart failure exhibits remarkable pathophysiologic heterogeneity. A large body of evidence suggests that regardless of the underlying etiology, heart failure is associated with induction of cytokines and chemokines that may contribute to the pathogenesis of adverse remodeling, and systolic and diastolic dysfunction. The pro-inflammatory cytokines tumor necrosis factor (TNF)-α, interleukin (IL)-1, and IL-6 have been extensively implicated in the pathogenesis of heart failure. Inflammatory cytokines modulate phenotype and function of all myocardial cells, suppressing contractile function in cardiomyocytes, inducing inflammatory activation in macrophages, stimulating microvascular inflammation and dysfunction, and promoting a matrix-degrading phenotype in fibroblasts. Moreover, cytokine-induced growth factor synthesis may exert chronic fibrogenic actions contributing to the pathogenesis of heart failure with preserved ejection fraction (HFpEF). In addition to their role in adverse cardiac remodeling, some inflammatory cytokines may also exert protective actions on cardiomyocytes under conditions of stress. Chemokines, such as CCL2, are also upregulated in failing hearts and may stimulate recruitment of pro-inflammatory leukocytes, promoting myocardial injury, fibrotic remodeling, and dysfunction. Although experimental evidence suggests that cytokine and chemokine targeting may hold therapeutic promise in heart failure, clinical translation remains challenging. This review manuscript summarizes our knowledge on the role of TNF-α, IL-1, IL-6, and CCL2 in the pathogenesis of heart failure, and discusses the promises and challenges of targeted anti-cytokine therapy. Dissection of protective and maladaptive cellular actions of cytokines in the failing heart, and identification of patient subsets with overactive or dysregulated myocardial inflammatory responses are required for design of successful therapeutic approaches.
Related collections
Most cited references114
- Record: found
- Abstract: found
- Article: not found
Overview of the IL-1 family in innate inflammation and acquired immunity.
- Record: found
- Abstract: found
- Article: not found
The inflammatory response in myocardial injury, repair, and remodelling.
- Record: found
- Abstract: found
- Article: not found
