- Record: found
- Abstract: found
- Article: found
Longitudinal SARS-CoV-2 humoral response in MS patients with and without SARS-CoV-2 infection prior to vaccination
Read this article at
Abstract
Introduction
During the COVID-19 pandemic, certain disease modifying therapies (DMTs) used in multiple sclerosis (MS), such as anti-CD20 therapies, have been associated with decreased humoral responses after SARS-CoV-2 vaccination. Hybrid immunity, referring to immunity after both vaccination and SARS-CoV-2 infection might increase humoral responses.
Methods
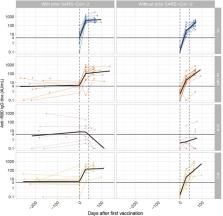
This was a substudy of two prospective cohort studies on SARS-CoV-2 antibodies after SARS-CoV-2 infection and vaccination. RBD-specific IgG titers of patients with MS and healthy controls who had experienced SARS-CoV-2 infection prior to the first vaccination were compared with those patients and healthy controls without prior infection. Humoral responses were measured at various time points after SARS-CoV-2 infection in convalescent patients and all patients prior to the first vaccination, 28 days after the first vaccination, and 28 days after the second vaccination.
Results
One hundred and two individuals [of which 34 patients with MS and DMTs (natalizumab or ocrelizumab), 30 patients without DMTs, and 38 healthy controls] were included. Fifty one of these individuals were convalescent. Median SARS-CoV-2 antibody titers were higher after the first vaccination in convalescent individuals compared with individuals without infection prior to vaccination. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibody titers were comparable after the second vaccination in patients with MS with and without prior infection. However, in the convalescent ocrelizumab-treated patients, SARS-CoV-2 antibody titers did not increase after vaccinations.
Conclusion
In patients with MS without anti-CD20 therapies, SARS-CoV-2 infection before vaccination increases humoral responses after the first vaccination, similar to the healthy controls. In patients with MS treated with ocrelizumab (convalescent and non-convalescent), humoral responses remained low.
Related collections
Most cited references10

- Record: found
- Abstract: found
- Article: found
Humoral- and T-Cell–Specific Immune Responses to SARS-CoV-2 mRNA Vaccination in Patients With MS Using Different Disease-Modifying Therapies

- Record: found
- Abstract: found
- Article: found
Hybrid immunity improves B cells and antibodies against SARS-CoV-2 variants
- Record: found
- Abstract: found
- Article: not found