- Record: found
- Abstract: found
- Article: found
Papulonecrotic Tuberculid
research-article

Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
A 30-year-old man presented with a 6 year history of recurrent, multiple asymptomatic
raised lesions over his back and bilateral upper limbs. He had been treated repeatedly
for a case of recurrent boils with oral and topical antibiotics. Some of the lesions
had healed spontaneously leaving behind unsightly scars. The patient denied any history
of associated fever, chronic cough, weight loss, and drug intake prior to the onset
of lesions. There was no recognized contact with tuberculosis patients. General and
systemic examination was essentially normal. Dermatological examination revealed the
presence of multiple, well-defined, hyperpigmented crusted papules of 0.5–1.0 cm in
size, distributed symmetrically over his entire back, extensor surface of bilateral
forearm, arm, and bilateral dorsum of foot, interspersed with atrophic varioliform
scarring (Figures 1 and 2). Routine laboratory workup was normal. Tuberculin (Mantoux)
was strongly positive at 72 hours (23 × 23 mm) with central necrosis (Figure 3). Sputum
for acid fast bacilli culture, chest radiograph, ultrasound abdomen, and pelvis did
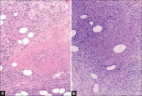
not reveal any abnormality. A biopsy specimen taken from a crusted papule over his
forearm (Figure 4) showed fibrinoid necrosis, surrounded by mixed inflammatory infiltrate
filling the entire dermis along with a few ill-defined epitheloid granulomas and lymphocytoclastic
vasculitis. These are consistent with papulonecrotic tuberculid.
Figure 1.
Multiple, hyperpigmented, crusted papules with varioliform scarring seen over the
back.
Figure 2.
Atrophic varioliform scarring over extensor aspect of left forearm.
Figure 3.
Positive Mantoux reaction (23 × 23).
Figure 4.
Single, crusted papule from which skin biopsy was taken.
The patient was started on a four drug combination therapy of rifampicin, isoniazid,
pyrazinamide, and ethambutol for two months initially followed by a combination of
rifampicin and isoniazid to complete a total of 6 months of standard antitubercular
therapy. The patient responded well and all of the lesions eventually healed.
Tuberculids are hypersensitivity reactions to Mycobacterium tuberculosis or its products
in individuals with good immunity.
1
Papulonecrotic tuberculid is a relatively uncommon manifestation of cutaneous tuberculosis.
2
It presents as chronic, recurrent, symmetrical eruption of necrotizing papules that
ulcerate, crust, and heal after a few weeks with varioliform scarring.
3
Hallmarks of this disease include positive mantoux test, evidence of present or past
tuberculosis, inability to isolate M. tuberculosis in the skin lesions, resolution
of lesions with atrophic varioliform lesions, and response to antitubercular therapy.
1
In a country like India where the prevalence of tuberculosis is high, existence of
papulonecrotic tuberculid is possible and the focus of the infection may not be demonstrable
in the majority of cases. Once diagnosed patients respond very well to antituberculosis
therapy. It is important to consider papulonecrotic tuberculid as a differential diagnosis
in any patient with recurrent eruption that heals with scarring in an endemic area.
Related collections
Most cited references3

- Record: found
- Abstract: found
- Article: found
Papulonecrotic Tuberculid with Positive Acid-fast Bacilli
Ren Jun, Liu Xiao-kun, Pan Chao … (2013)