- Record: found
- Abstract: found
- Article: found
Brief Report: Virologic Impact of the Dolutegravir Transition: Prospective Results From the Multinational African Cohort Study
Read this article at
Background:
The real-world impact on viral suppression of switching from non–dolutegravir-based therapy to tenofovir/lamivudine/dolutegravir (TLD) is not thoroughly characterized in Africa. We described the virologic consequences of switching regimens in the African Cohort Study (AFRICOS), an observational cohort in Nigeria, Kenya, Uganda, and Tanzania.
Methods:
Among antiretroviral-experienced people living with HIV (PLWH) in AFRICOS, we compared viral load (VL) nonsuppression (VL ≥ 1000 copies/mL) among those who switched with those who never switched to TLD, restricting to participants who had at least 1 visit with a recorded VL after the countrywide rollout of TLD. We calculated Kaplan–Meier curves and conducted Cox proportional hazards modeling to estimate adjusted hazard ratios and 95% confidence intervals for factors potentially associated with nonsuppression.
Results:
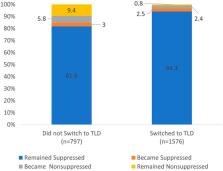
As of September 1, 2021, there were 3108 PLWH enrolled. Among 1576 participants who switched to TLD, 1486 (94.3%) remained suppressed after transition, 12 (0.8%) remained unsuppressed, and 38 (2.4%) lost suppression, compared with 652 (82.1%), 75 (9.4%), and 46 (5.8%), respectively, of 797 participants who did not switch ( P < 0.001). After adjustment for sex, age, study site, and self-reported antiretroviral therapy adherence, virally suppressed participants who did not switch to TLD had significantly higher rates of losing viral suppression compared with those who switched (adjusted hazard ratio: 4.26; 95% confidence interval: 2.72 to 6.68).
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
Dolutegravir plus abacavir-lamivudine for the treatment of HIV-1 infection.
- Record: found
- Abstract: found
- Article: not found
Dolutegravir plus Two Different Prodrugs of Tenofovir to Treat HIV
- Record: found
- Abstract: found
- Article: not found