- Record: found
- Abstract: found
- Article: found
A pragmatic randomized control trial and realist evaluation on the implementation and effectiveness of an internet application to support self-management among individuals seeking specialized mental health care: a study protocol
Read this article at
Abstract
Background
Mental illness is a substantial and rising contributor to the global burden of disease. Access to and utilization of mental health care, however, is limited by structural barriers such as specialist availability, time, out-of-pocket costs, and attitudinal barriers including stigma. Innovative solutions like virtual care are rapidly entering the health care domain. The advancement and adoption of virtual care for mental health, however, often occurs in the absence of rigorous evaluation and adequate planning for sustainability and spread.
Methods
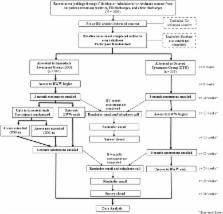
A pragmatic randomized controlled trial with a nested comparative effectiveness arm, and concurrent realist process evaluation to examine acceptability, effectiveness, and cost-effectiveness of the Big White Wall (BWW) online platform for mental health self-management and peer support among individuals aged 16 and older who are accessing mental health services in Ontario, Canada. Participants will be randomized to 3 months of BWW or treatment as usual. At the end of the 3 months, participants in the intervention group will have the opportunity to opt-in to an intervention extension arm. Those who opt-in will be randomized to receive an additional 3 months of BWW or no additional intervention. The primary outcome is recovery at 3 months as measured by the Recovery Assessment Scale-revised (RAS-r). Secondary outcomes include symptoms of depression and anxiety measured with the Personal Health Questionnaire-9 item (PHQ-9) and the Generalized Anxiety Disorder Questionnaire-7 item (GAD-7) respectively, quality of life measured with the EQ-5D-5L, and community integration assessed with the Community Integration Questionnaire. Cost-effectiveness evaluations will account for the cost of the intervention and direct health care costs. Qualitative interviews with participants and stakeholders will be conducted throughout.
Discussion
Understanding the impact of virtual strategies, such as BWW, on patient outcomes and experience, and health system costs is essential for informing whether and how health system decision-makers can support these strategies system-wide. This requires clear evidence of effectiveness and an understanding of how the intervention works, for whom, and under what circumstances. This study will produce such effectiveness data for BWW, while simultaneously exploring the characteristics and experiences of users for whom this and similar online interventions could be helpful.
Trial registration
Clinicaltrials.gov NCT02896894. Registered on 31 August 2016 (retrospectively registered).
Related collections
Most cited references22
- Record: found
- Abstract: found
- Article: not found
Monitoring depression treatment outcomes with the patient health questionnaire-9.
- Record: found
- Abstract: found
- Article: not found
Efficacy of peer support interventions for depression: a meta-analysis.
- Record: found
- Abstract: found
- Article: not found