- Record: found
- Abstract: found
- Article: found
Data resource profile: Clinical Practice Research Datalink (CPRD) Aurum
research-article
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Data resource basics
Clinical Practice Research Datalink (CPRD) is a UK government, not-for-profit research
service that has been supplying anonymized primary care data for public health research
for more than 30 years. In October 2017 CPRD launched a new data resource called CPRD
Aurum. CPRD Aurum is a database containing routinely collected data from primary care
practices in England, capturing diagnoses, symptoms, prescriptions, referrals and
tests for over 19 million patients as of September 2018 (Figure 1). Primary care data
in CPRD Aurum have been linked to national secondary care databases as well as deprivation
and death registration data (Table 1).
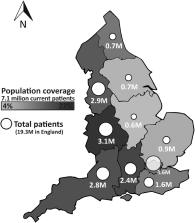
Figure 1.
CPRD Aurum population coverage and total patients by English region, September 2018.
Circles represent total patients in CPRD Aurum in each region. Shading represents
population coverage of current patients as a proportion of total regional population.
Table 1.
Key details about CPRD Aurum
UK countries covered
Consenting practices in England (consenting practices from Northern Ireland available
from 2019)
Who is included?
19 million patients from 738 practices (10% of English practices), of whom 7 million
were alive and currently contributing (13% of the population of England)
What is recorded?
Demographics, diagnoses, symptoms, prescriptions, referrals, immunizations, lifestyle
factors, tests and results
Start and end dates
From 1995
a
to September 2018, with a median follow-up of 4.2 years (IQR: 1.5–11.4) for all patients
and 9.1 years (IQR: 3.3–20.1) for current patients. CPRD Aurum is updated on a monthly
basis.
Standard linkages
Hospital Episode Statistics, Death Registration, Cancer data, Mental Health Services
Dataset, Small Area-Level Data (deprivation measures and rural–urban classification)
a
This is an arbitrary cut-off and the database includes records pre-dating 1995, however,
the completeness of recorded information following this point is expected to be more
reliable.
IQR, interquartile range.
UK primary care
The United Kingdom’s (UK) National Health Service (NHS) is a publicly funded health
service, free at the point of use. General practitioners (GPs) are considered the
‘gatekeepers’ of the NHS, referring patients to secondary care and diagnostic tests.
1
Over 98% of the population is registered at one of the 7300 GP practices in England.
2
A unique patient identifier, the NHS number, is used in primary, secondary and tertiary
care settings, enabling linkages to other data sources.
3
There are four principal GP IT systems (primary care patient management software system)
suppliers in England
4
and the largest coverage is provided by EMIS Health® (EMIS Web® software is used in
56% of English practices).
5
CPRD Aurum, discussed in this Data Resource Profile, encompasses EMIS Web® GP practices
that have agreed to contribute data to this database on a daily basis. CPRD also collects
data from practices using Vision® software that contribute to the CPRD GOLD database,
which has been used in epidemiological research for 30 years.
6
CPRD Aurum
CPRD Aurum includes patient electronic healthcare records (EHR) collected routinely
in primary care. When a practice agrees to contribute patient data to CPRD Aurum,
CPRD receives a full historic collection of the coded part of the practice’s electronic
health records, which includes data on deceased patients and those who have left the
practice. Since 25 May 2018, individuals in England can opt-out of sharing their confidential
patient information for research purposes
7
and, as of 1 September 2018, 2.7% of the English primary care registered population
had opted-out.
8
As of September 2018, CPRD Aurum included 7 million patients who were alive and registered
at EMIS Web® currently contributing practices (Table 2), representing around 13% of
the population of England. This number will increase as additional practices sign-up
as contributors to this data resource as part of an ongoing recruitment strategy.
Consenting practices from Northern Ireland will start contributing data to CPRD Aurum
from 2019.
Table 2.
Demographic characteristics of Aurum patients, September 2018
All patients
Current
No. patients (practices)
19 305 234 (738)
7 125 786 (731)
Gender
Male
9 309 928 (48.2%)
3 552 291 (49.9%)
Female
9 994 725 (51.8%)
3 573 360 (50.1%)
Indeterminate
581 (<0.01%)
135 (<0.01%)
Age in 2018
<18
−
1 427 297 (20.0%)
18–64
−
4 463 385 (62.6%)
65+
−
1 235 104 (17.3%)
English Region
North East
741 657 (3.8%)
327 786 (4.6%)
North West
2 948 404 (15.3%)
1 186 522 (16.7%)
Yorkshire & The Humber
715 487 (3.7%)
262 132 (3.7%)
East Midlands
551 130 (2.9%)
186 831 (2.6%)
West Midlands
3 126 234 (16.2%)
1 298 818 (18.2%)
East of England
889 553 (4.6%)
356 308 (5.0%)
South West
2 781 559 (14.4%)
980 184 (13.8%)
South Central
2 359 844 (12.2%)
847 481 (11.9%)
London
3 623 487 (18.8%)
1 125 905 (15.8%)
South East Coast
1 567 879 (8.1%)
553 819 (7.8%)
Follow-up since 1995a (median years, IQR)
4.2 (1.5–11.4)
9.1 (3.3–20.1)
‘Current’ refers to patients who are alive and registered at actively contributing
practices. IQR, interquartile range. aThe database includes records pre-dating 1995.
Key demographic information on current and total patients is presented in Table 2.
Median follow-up since 1995 for all patients was 4.2 years [interquartile range (IQR):
1.5–11.4] and 9.1 years (3.3–20.1) for current patients. For patients in CPRD Aurum,
the mean decile on the 2015 Index of Multiple Deprivation
9
was 5.3 (1 being the least deprived) compared with the mean decile in England (of
5.5), suggesting a slightly less deprived population in the database.
Linkage to other datasets
Data from patients from all practices in CPRD Aurum can be linked to a range of health-related
data sources including secondary care, disease registries and death registration records
(Table 3). CPRD Aurum are linked to other patient-level health data by a trusted third
party, NHS Digital, using NHS number, exact date of birth, sex and patient residence
postcode (linkage methodology details are described in Padmanabhan et al., 2018).
10
CPRD does not receive or hold patient identifiers including name, full date of birth,
postcode and NHS number. Identifiers are removed prior to transfer of data to CPRD
to protect patient confidentiality. Personal identifiers are sent separately from
GP practices to NHS Digital, the statutory body in England able to receive patient
identifiable data, to enable linkage.
Table 3.
Standard linkages with CPRD Aurum data
Linkage dataset
Coveragea
Key information (including coding/scoring system)
ONS Death Registration Data
1998–2018
Date, place, and causes of death (ICD)
Hospital Episode Statistics (HES)
Admitted Patient Care
1997–2017
Diagnoses (ICD) and procedures (OPCS)
Outpatient
2003–2017
Diagnoses (ICD) data
Accident & Emergency
2007–2017
Diagnoses (A&E codes) data
Diagnostic Imaging Dataset
2012–2017
Imaging tests data
PROM
2009–2017
Quality of life & condition-specific scales
National Cancer Registration and Analysis Service
Cancer registration
1990–2015
Diagnoses (ICD) and tumour site
Systemic Anti-Cancer Treatment
2014–2015
Procedures and outcomes (ICD & OPCS)
National Radiotherapy Dataset
2012–2015
Procedures (ICD & OPCS)
Cancer Patient Experience Survey
2010–2013
Self-reported cancer patient data
Mental Health Services Data Set
2007–2015
Diagnoses (ICD), functioning (HoNOS)
Small area-level data
Index of Multiple Deprivation
2004–2015
Patient or practice data, including domains
Townsend Index
2001
Patient-level deprivation data
Carstairs Index
2011
Practice-level deprivation data
Rural Urban Classification
2011
Practice-level classification
PROM, Patient Reported Outcome Measures; ICD, WHO International Classification of
Diseases; OPCS, Office of Population Censuses and Surveys Classification of Surgical
Operations and Procedures; HoNOS, Health of the Nation Outcome Scale.
a
Coverage is updated regularly based on data-provider releases. For up to date information
on available linkages, visit cprd.com/linked-data
Primary care data in CPRD Aurum have been linked to Office for National Statistics
Death Registration Data,
11
which are considered the gold standard for mortality data in the UK and contain the
date, place and cause of death.
12
The Hospital Episode Statistics (HES) datasets include Admitted Patient Care (APC)
data which contain details of all admissions to, or attendances at English NHS health
care providers, including acute hospital trusts, primary care trusts and mental health
trusts.
13
HES Outpatient (OP) contains records of outpatient appointments in England including
dates, specialty, clinical diagnoses and procedures.
14
HES Accident and Emergency (A&E) consists of individual records of patient care administered
in the accident and emergency setting in England, also including diagnoses and procedures.
15
The HES Diagnostic Imaging Dataset (DID) contains information about diagnostic imaging
tests conducted, such as X-rays and MRI scans, taken from NHS radiological information
systems.
16
Cancer data provided by Public Health England (PHE) via the National Cancer Registration
and Analysis Service (NCRAS)
17
have also been linked to CPRD Aurum. Linked NCRAS CPRD datasets include Cancer Registration
data (record for each registrable tumour diagnosed or treated in England), the Systemic
Anti-Cancer Treatment Dataset (SACT; chemotherapy treatment and outcome), the National
Radiotherapy Dataset (RTDS; radiotherapy records for cancer, including teletherapy
and brachytherapy) and the Cancer Patient Experience Survey (CPES; four waves of self-reported
patient data).
CPRD Aurum data has also been linked to the Mental Health Services Dataset (MHDS),
which contains records of individuals who accessed secondary care adult, and child
and adolescent mental health services, including diagnoses and episodes of care. Small
area-level linkages on practice or patients’ residence postcodes include several measures
of area-level deprivation (Index of Multiple Deprivation,
9
Townsend Index,
18
and Carstairs Index
19
) and practice-level rural–urban classification.
20
Data collected
CPRD Aurum is a dynamic database, and data are collected from contributing practices
on a daily basis and processed to create monthly snapshots for observational research.
This full de-identified coded clinical record includes symptoms, diagnoses, prescriptions,
immunizations, tests, lifestyle factors and referrals recorded by the GP or other
practice staff, but does not include free text medical notes.
Structure
The database structure is based on eight separate files, each containing patients’
pseudonymized identifiers (Figure 2). The patient file records basic patient demographics,
date of death if applicable and details on when the patient registered/deregistered
from the practice. The practice file contains the practice region and the most recent
date of data collection for the practice, and the staff file contains the job category
for each staff member in CPRD Aurum. The consultation file holds information relating
to the type of consultation as entered by the GP (e.g. telephone, home visit, practice
visit), which can be internally linked (within CPRD Aurum) to observations that occur
during the consultation via the consultation identifier, and to the staff member that
conducted the consultation via the staff file.
Figure 2.
CPRD Aurum dataset structure. 1Includes symptoms, diagnoses, immunizations, tests
and lifestyle factors. Note: the problem and referral tables contain add-on information
for certain types of observations. Some consultations are linked to observations.
Some drug issues are linked to problem-type observations.
The observation file contains the medical-history data entered on the GP system including
symptoms, clinical measurements, laboratory test results, and diagnoses, as well as
demographic information recorded as a clinical code (e.g. patient ethnicity). Observations
that occur during a consultation are linked via the consultation identifier. CPRD
Aurum data are structured in a long format (multiple rows per subject), and observations
are linked to a parent observation. For example, measurements of systolic and diastolic
blood pressure will be grouped together via a parent observation for blood pressure
measurement.
Data in the referral and problem files are linked to the observation file and contain
‘add-on’ data for referral-type and problem-type observations. The referral file contains
information involving both inbound and outbound patient referrals to or from external
care centres (most frequently from the practice to a secondary care provider). The
problem file contains details of the patient’s medical history that have been defined
by the GP as a ‘problem’, including the significance of the problem and its expected
duration. GPs may use ‘problems’ to manage chronic conditions, thus enabling them
to group clinical events (including drug prescriptions, measurements and symptoms)
by problem rather than chronologically by consultation date. Finally, the drug-issue
file contains data relating to all prescriptions (for drugs and devices) issued by
the GP and are linked back to problem-type observations.
Coding
CPRD provides data dictionaries and code browsers to identify relevant codes in CPRD
Aurum. The Medical Dictionary contains information on all medical history observations
that have been recorded. Observations are coded using a combination of SNOMED CT (UK
edition),
21
Read Version 2
22
and local EMIS Web® codes. The Drug Dictionary contains information on drug and device
prescriptions recorded in EMIS Web®. This information is coded using the Dictionary
of Medicines and Devices (dm+d), which exists within the SNOMED CT terminological
structure.
23
Practice staff are able to add additional information to patient records as free text.
However, for data governance reasons, CPRD does not collect free text as these fields
may contain identifiable patient information.
Ethics
CPRD obtains annual research ethics approval from the UK’s Health Research Authority
(HRA) Research Ethics Committee (REC) (East Midlands – Derby, REC reference number
05/MRE04/87) to receive and supply patient data for public health research. Therefore,
no additional ethics approval is required for observational studies using CPRD Aurum
data for public health research, subject to individual research protocols meeting
CPRD data governance requirements.
Funding
CPRD is jointly sponsored by the UK government’s Medicines and Healthcare products
Regulatory Agency and the National Institute for Health Research (NIHR). As a not-for-profit
UK government body, CPRD seeks to recoup the cost of delivering its research services
to academic, industry and government researchers through research user licence fees.
Data resource use
As CPRD Aurum is a relatively recent data resource, no studies have been published
to date. Nevertheless, since the recent launch of CPRD Aurum a number of approved
research projects are already underway – including in pharmacovigilance, drug prescribing
patterns, health services and policy evaluation, and disease risk factors. For instance,
an ongoing academic research study is looking at patient treatment pathways in primary
and secondary care using linked hospital and clinical audit data. A pharmacovigilance
study is using CPRD Aurum and linked hospital data to examine the association between
common drug therapies and heart arrhythmia. CPRD GOLD, which contains comparable NHS
GP data to CPRD Aurum (but based on practices using a different GP IT system) has
been used extensively in over 2000 publications that illustrate the potential research
applications of CPRD Aurum.
24
A bibliography of all peer-reviewed published studies using CPRD data, dating back
over the past 30 years, is available on the CPRD website (www.cprd.com/bibliography).
Strengths and weaknesses
With records on over 19 million patients as of September 2018, CPRD Aurum contains
a wide range of diagnostic, prescription, procedure and lifestyle information. The
key strengths of CPRD Aurum are its size and coverage, longitudinal follow-up, representativeness,
standard linkages and data quality assurance processes.
Strengths
Database size and representativeness
The data currently cover 13% of the population of England, and are representative
of the broader English population in terms of geographical spread (Figure 1) and deprivation
(median decile on index of multiple deprivation (IMD) of 5.3), as well as age and
gender [see Figure 3 comparing mid-2017 CPRD Aurum to mid-2017 data published by the
Office for National Statistics (ONS)].
25
Figure 3.
Population pyramids for CPRD Aurum and ONS data. Based on mid-2017 ONS and mid-2017
CPRD Aurum data.
Data linkages
Patient-level data have been linked to secondary care and other data sets, providing
a fuller picture of the patient care pathway and outcomes. All CPRD Aurum practices
have consented to participating in the linkage scheme, which includes data from national
secondary care databases (hospitals and mental health service providers), the national
cancer registry, death registrations and deprivation measures (Table 3).
Data quality assurance processes
CPRD undertakes various levels of validation and quality assurance on the daily GP
data collection comprising over 900 checks covering the integrity, structure and format
of the data. Issues highlighted by the checks are reviewed and addressed before data
is incorporated into CPRD Aurum.
Collection-level validation ensures integrity by checking that data received from
EMIS Web® practices contain only expected data files and ensures that all data elements
are of the correct type, length and format. Duplicate records are identified and removed.
Transformation-level validation checks for referential integrity between records to
ensure that there are no orphan records included in CPRD Aurum (e.g. that all event
records link to a patient). Research-quality-level validation is the last level and
covers the actual content of the data. CPRD provides a patient-level data quality
metric in the form of a binary ‘acceptability’ flag. This is based on recording and
internal consistency of key variables including date of birth, practice registration
date and transfer out date.
Separately, a derived death date (consolidating death-related information captured
in different parts of the patient record) is currently undergoing validation against
both GP-recorded and official ONS death records, and a practice-level quality metric
(ascertaining temporal gaps in recording quality) is in development that will be added
to future builds of CPRD Aurum.
Weaknesses
Missing data
Though secondary care data, including key diagnoses, can be manually recorded by GPs,
this information is often incomplete in primary care records. Additional data may
be available in free text entries or letters received by GPs from secondary care facilities,
but this is not available to CPRD or researchers for data governance reasons. However,
additional information on patient pathways can be obtained through linkage to other
data sources as described above. Data on prescriptions for medications and devices
that have been issued in primary care are very reliable, however, information on medications
dispensed, secondary care prescriptions and over-the-counter use are not recorded
in primary care.
GP IT systems and coding
Possible variations in coding between practices and over time, as well as the current
transition to SNOMED coding,
21
should be considered by researchers when planning a study using CPRD Aurum. Additionally,
the database structure of CPRD Aurum differs somewhat from other UK databases, including
CPRD GOLD,
6
due to underlying differences between EMIS Web® and Vision® software structures, which
may affect data comparability. CPRD has published preliminary guidance for researchers
on differences between the CPRD GOLD and CPRD Aurum databases.
26
Data resource access
Researchers can apply for a limited licence to access CPRD data for public health
research, subject to individual research protocols meeting CPRD data governance requirements.
CPRD Aurum data is provided in tab-delimited text files and can be imported into any
standard statistical software package. As a not-for-profit organization, CPRD recoups
its costs through research user licence fees (annual multi-study license or dataset-specific
license), with additional fees for linkage to other datasets.
More details including the data specification, applications process, and access to
linked data, are available on the CPRD website (https://www.cprd.com). Researchers
can also request feasibility counts from CPRD to inform sample-size estimates and
decisions regarding suitability of CPRD Aurum for their proposed research. Any other
queries can be directed to CPRD Enquiries [enquiries@cprd.com].
Profile in a nutshell
CPRD Aurum is a UK primary care database set up for public health research and benefit,
updated monthly for observational research, with standard linkages to hospital, mortality,
cancer, mental health and deprivation data.
As of September 2018, 738 GP practices in England have contributed data, which included
19 million patients, of whom over 7 million were currently registered at contributing
practices.
De-identified coded primary care data are collected from GP practices that have consented
to provide data to CPRD Aurum.
Symptoms, diagnoses, prescriptions, immunizations, tests and lifestyle factors are
recorded by the GP or other practice staff, and CPRD Aurum has been linked to additional
secondary care databases.
Access to data for public health research is subject to data governance requirements
and contractual obligations being met. Queries can be directed to CPRD Enquiries (enquiries@cprd.com).
Conflict of interest: None declared.
Related collections
Most cited references5

- Record: found
- Abstract: found
- Article: found
Data Resource Profile: Hospital Episode Statistics Admitted Patient Care (HES APC)
Annie Herbert, Linda Wijlaars, Ania Zylbersztejn … (2017)

- Record: found
- Abstract: found
- Article: found
Approach to record linkage of primary care data from Clinical Practice Research Datalink to other health-related patient data: overview and implications
Shivani Padmanabhan, Lucy Carty, Ellen Cameron … (2018)
