- Record: found
- Abstract: found
- Article: found
How long do nosocomial pathogens persist on inanimate surfaces? A systematic review
Read this article at
Abstract
Background
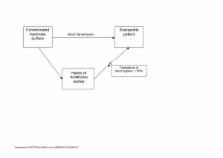
Inanimate surfaces have often been described as the source for outbreaks of nosocomial infections. The aim of this review is to summarize data on the persistence of different nosocomial pathogens on inanimate surfaces.
Methods
The literature was systematically reviewed in MedLine without language restrictions. In addition, cited articles in a report were assessed and standard textbooks on the topic were reviewed. All reports with experimental evidence on the duration of persistence of a nosocomial pathogen on any type of surface were included.
Results
Most gram-positive bacteria, such as Enterococcus spp. (including VRE), Staphylococcus aureus (including MRSA), or Streptococcus pyogenes, survive for months on dry surfaces. Many gram-negative species, such as Acinetobacter spp., Escherichia coli, Klebsiella spp., Pseudomonas aeruginosa, Serratia marcescens, or Shigella spp., can also survive for months. A few others, such as Bordetella pertussis, Haemophilus influenzae, Proteus vulgaris, or Vibrio cholerae, however, persist only for days. Mycobacteria, including Mycobacterium tuberculosis, and spore-forming bacteria, including Clostridium difficile, can also survive for months on surfaces. Candida albicans as the most important nosocomial fungal pathogen can survive up to 4 months on surfaces. Persistence of other yeasts, such as Torulopsis glabrata, was described to be similar (5 months) or shorter ( Candida parapsilosis, 14 days). Most viruses from the respiratory tract, such as corona, coxsackie, influenza, SARS or rhino virus, can persist on surfaces for a few days. Viruses from the gastrointestinal tract, such as astrovirus, HAV, polio- or rota virus, persist for approximately 2 months. Blood-borne viruses, such as HBV or HIV, can persist for more than one week. Herpes viruses, such as CMV or HSV type 1 and 2, have been shown to persist from only a few hours up to 7 days.
Related collections
Most cited references162
- Record: found
- Abstract: found
- Article: not found
Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation.
- Record: found
- Abstract: found
- Article: not found
Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs.
- Record: found
- Abstract: found
- Article: not found