- Record: found
- Abstract: found
- Article: found
Contemporary Trends in Hospitalizations for Comorbid Chronic Liver Disease and Substance Use Disorders
Read this article at
Abstract
INTRODUCTION:
Chronic liver diseases (CLDs) and substance use disorders (SUDs) are increasingly prevalent and often coexist. Contemporary studies describing the characteristics and hospitalization trends of those with comorbid CLD-SUD are lacking. We aimed to characterize a population-based cohort with comorbid CLD-SUD and describe trends in these hospitalizations over time by individual-level characteristics.
METHODS:
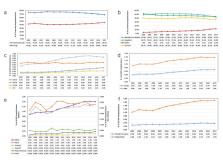
We performed a cross-sectional analysis of the National Inpatient Sample from 2005 through 2017. Diagnosis codes were used to identify adult hospitalizations with CLD, SUD, or both. Bivariate and multivariate analyses were used to make comparisons between diagnosis categories. Unadjusted and age-adjusted trends in these hospitalizations were described over time.
RESULTS:
Of 401,867,749 adult hospital discharges, 3.2% had CLD-only and 1.7% had comorbid CLD-SUD. Compared with CLD-only, comorbid CLD-SUD hospitalizations resulted in higher inpatient mortality (3.1% vs 2.4%, P < 0.001) and were associated with younger age, male sex, Native American race, and urban and Western US location. Over time, comorbid hospitalizations grew 34%, and the demographics shifted with larger increases in hospitalization rates seen in younger individuals, women, Native Americans, and those publicly insured. In comorbid hospitalizations, alcoholic SUD and CLD decreased, but drug SUDs and nonalcoholic fatty liver diseases are fast-growing contributors.
DISCUSSION:
In this comprehensive analysis of US hospitalizations, comorbid CLD-SUD hospitalizations are increasing over time and lead to higher inpatient mortality than CLD alone. We further characterize the changing demographics of these hospitalizations, providing a contemporary yet inclusive look at comorbid CLD-SUD hospitalizations. These data can guide interventions needed to improve the poor outcomes suffered by this growing population.
Related collections
Most cited references54
- Record: found
- Abstract: found
- Article: not found
Contemporary Epidemiology of Chronic Liver Disease and Cirrhosis

- Record: found
- Abstract: found
- Article: found
Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study

- Record: found
- Abstract: found
- Article: found