- Record: found
- Abstract: found
- Article: found
The Hoorn Diabetes Care System (DCS) cohort. A prospective cohort of persons with type 2 diabetes treated in primary care in the Netherlands
Read this article at
Abstract
Purpose
People with type 2 diabetes (T2D) have a doubled morbidity and mortality risk compared with persons with normal glucose tolerance. Despite treatment, clinical targets for cardiovascular risk factors are not achieved. The Hoorn Diabetes Care System cohort (DCS) is a prospective cohort representing a comprehensive dataset on the natural course of T2D, with repeated clinical measures and outcomes. In this paper, we describe the design of the DCS cohort.
Participants
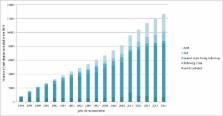
The DCS consists of persons with T2D in primary care from the West-Friesland region of the Netherlands. Enrolment in the cohort started in 1998 and this prospective dynamic cohort currently holds 12 673 persons with T2D.
Findings to date
Clinical measures are collected annually, with a high internal validity due to the centrally organised standardised examinations. Microvascular complications are assessed by measuring kidney function, and screening feet and eyes. Information on cardiovascular disease is obtained by 1) self-report, 2) electrocardiography and 3) electronic patient records. In subgroups of the cohort, biobanking and additional measurements were performed to obtain information on, for example, lifestyle, depression and genomics. Finally, the DCS cohort is linked to national cancer and all-cause mortality registers. A selection of published findings from the DCS includes identification of subgroups with distinct development of haemoglobin A1c, blood pressure and retinopathy, and their predictors; validation of a prediction model for personalised retinopathy screening; the assessment of the role of genetics in development and treatment of T2D, providing options for personalised medicine.
Future plans
We will continue with the inclusion of persons with newly diagnosed T2D, follow-up of persons in the cohort and linkage to morbidity and mortality registries. Currently, we are involved in (inter)national projects on, among others, biomarkers and prediction models for T2D and complications and we are interested in collaborations with external researchers.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
Development and validation of the Patient Assessment of Chronic Illness Care (PACIC).
- Record: found
- Abstract: found
- Article: not found