- Record: found
- Abstract: found
- Article: found
Tranexamic acid for treatment and prophylaxis of bleeding and hyperfibrinolysis
Read this article at
Summary
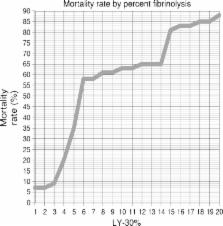
Uncontrolled massive bleeding with subsequent derangement of the coagulation system is a major challenge in the management of both surgical and seriously injured patients. Under physiological conditions activators and inhibitors of coagulation regulate the sensitive balance between clot formation and fibrinolysis. In some cases, excessive and diffuse bleeding is caused by systemic activation of fibrinolysis, i. e. hyperfibrinolysis (HF). Uncontrolled HF is associated with a high mortality. Polytrauma patients and those undergoing surgical procedures involving organs rich in plasminogen proactivators (e. g. liver, kidney, pancreas, uterus and prostate gland) are at a high risk for HF. Antifibrinolytics, such as tranexamic acid (TXA) are used for prophylaxis and treatment of bleeding caused by a local or generalized HF as well as other hemorrhagic conditions. TXA is a synthetic lysine analogue that has been available in Austria since 1966. TXA is of utmost importance in the prevention and treatment of traumatic and perioperative bleeding due to the resulting reduction in perioperative blood loss and blood transfusion requirements. The following article presents the different fields of application of TXA with particular respect to indications and dosages, based on a literature search and on current guidelines.
Related collections
Most cited references114
- Record: found
- Abstract: found
- Article: found
European Stroke Organization Guidelines for the Management of Intracranial Aneurysms and Subarachnoid Haemorrhage

- Record: found
- Abstract: found
- Article: found
The European guideline on management of major bleeding and coagulopathy following trauma: fourth edition
- Record: found
- Abstract: found
- Article: not found