- Record: found
- Abstract: found
- Article: found
Frequency of Red Cell Alloimmunization and Autoimmunization in Thalassemia Patients: A Report from Eastern India
Read this article at
Abstract
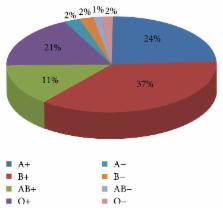
Introduction. Red blood cell (RBC) alloimmunization and autoimmunization remain a major problem in transfusion dependent thalassemic patients. There is a paucity of data on the incidence of RBC alloimmunization and autoimmunization in thalassemic patients from eastern part of India, as pretransfusion antibody screening is not routinely performed. Aims. To assess the incidence of RBC alloimmunization and autoimmunization in transfusion dependent thalassemic patients in eastern India. Materials and Methods. Total 500 thalassemia cases were evaluated. The antibody screening and identification were performed with commercially available panel cells (Diapanel, Bio-rad, Switzerland) by column agglutination method. To detect autoantibodies, autocontrol and direct antiglobulin tests were carried out using polyspecific coombs (IgG + C3d) gel cards in all patients. Results. A total of 28 patients developed RBC alloimmunization (5.6%) and 5 patients had autoantibodies (1%). Alloantibody against c had the highest incidence (28.57%) followed by E (21.42%). Five out of 28 (17.85%) patients had developed antibodies against both c and E. Conclusion. Data from this study demonstrate that the RBC alloantibody and autoantibody development rates are significant in our region. Thus, pretransfusion antibody screening needs to be initiated in eastern India in order to ensure safe transfusion practice.
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
Transfusion and alloimmunization in sickle cell disease. The Cooperative Study of Sickle Cell Disease.
- Record: found
- Abstract: found
- Article: not found
Clinical significance of RBC alloantibodies and autoantibodies in sickle cell patients who received transfusions.
- Record: found
- Abstract: found
- Article: not found