- Record: found
- Abstract: found
- Article: not found
Lethal pediatric cerebral vasculitis triggered by Severe Acute Respiratory Syndrome Coronavirus 2: a case report
Read this article at
Abstract
Objectives
We report the clinical, radiological, laboratory, and neuropathological findings in support of the first diagnosis of lethal, small-vessel cerebral vasculitis triggered by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in a pediatric patient.
Patient description
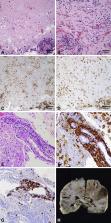
A previously healthy, 8-year-old Hispanic female presented with subacute onset left-sided weakness two weeks after a mild febrile illness. SARS-CoV-2 nasopharyngeal swab was positive. Magnetic resonance imaging (MRI) revealed an enhancing right frontal lobe lesion with significant vasogenic edema. Two brain biopsies of the lesion showed perivascular and intraluminal lymphohistiocytic inflammatory infiltrate consistent with vasculitis. Despite extensive treatment with immunomodulatory therapies targeting primary angiitis of the central nervous system, she experienced neurologic decline and died 93 days after presentation. SARS-CoV-2 testing revealed positive serum IgG and positive cerebrospinal fluid IgM. Comprehensive infectious, rheumatologic, hematologic/oncologic, and genetic evaluation did not identify an alternative etiology. Post-mortem brain autopsy remained consistent with vasculitis.
Discussion
This is the first pediatric presentation to suggest SARS-CoV-2 can lead to a fatal, post-infectious, inflammatory small-vessel cerebral vasculitis. Our case is unique in including supportive cerebrospinal fluid and post-mortem tissue analysis. While most children recover well from neurologic complications of SARS-CoV-2, we emphasize the potential mortality in a child with no risk factors for severe disease.
Related collections
Most cited references13
- Record: found
- Abstract: found
- Article: not found
Neurologic Involvement in Children and Adolescents Hospitalized in the United States for COVID-19 or Multisystem Inflammatory Syndrome
- Record: found
- Abstract: found
- Article: not found
Neuroimaging manifestations in children with SARS-CoV-2 infection: a multinational, multicentre collaborative study

- Record: found
- Abstract: found
- Article: found
