- Record: found
- Abstract: found
- Article: not found
The potential role of neopterin in Covid-19: a new perspective
Read this article at
Abstract
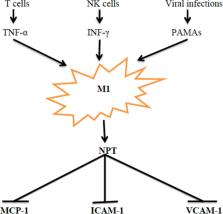
Neopterin (NPT) is a member of pteridines group, synthesized by macrophages when stimulated by interferon gamma (INF-γ). NPT is regarded as a macrophage stimulation indicator, marker of cellular immune activation and T helper 1 (Th1) type 1 immune response. Here, we aimed to provide a view point on the NPT features and role in Covid-19. Serum NPT level is regarded as an independent prognostic factor for Covid-19 severity, with levels starting to increase from the 3rd day of SARS-CoV-2 infection, being associated with severe dyspnea, longer hospitalization period and complications. Also, early raise of NPT reflects monocytes/macrophages activation before antibody immune response, despite the NPT level may also remain high in Covid-19 patients or at the end of incubation period before the onset of clinical symptoms. On the other hand , NPT attenuates the activity of macrophage foam cells and is linked to endothelial inflammation through inhibition of adhesion molecules and monocytes migration. However, NPT also exerts anti-inflammatory and antioxidant effects by suppressing NF-κB signaling and NLRP3 inflammasomes. NPT can be viewed as a protective compensatory mechanism to counterpoise hyper-inflammation, oxidative stress, and associated organ damage.
Related collections
Most cited references54
- Record: found
- Abstract: found
- Article: not found
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- Record: found
- Abstract: found
- Article: not found
ACUTE KIDNEY INJURY IN PATIENTS HOSPITALIZED WITH COVID-19
- Record: found
- Abstract: found
- Article: not found
