- Record: found
- Abstract: found
- Article: found
Blood-Brain Barrier Opening in Primary Brain Tumors with Non-invasive MR-Guided Focused Ultrasound: A Clinical Safety and Feasibility Study
Read this article at
Abstract
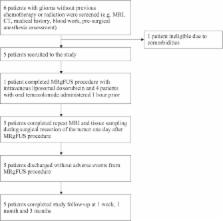
The blood-brain barrier (BBB) has long limited therapeutic access to brain tumor and peritumoral tissue. In animals, MR-guided focused ultrasound (MRgFUS) with intravenously injected microbubbles can temporarily and repeatedly disrupt the BBB in a targeted fashion, without open surgery. Our objective is to demonstrate safety and feasibility of MRgFUS BBB opening with systemically administered chemotherapy in patients with glioma in a phase I, single-arm, open-label study. Five patients with previously confirmed or suspected high-grade glioma based on imaging underwent the MRgFUS in conjunction with administration of chemotherapy (n = 1 liposomal doxorubicin, n = 4 temozolomide) one day prior to their scheduled surgical resection. Samples of “sonicated” and “unsonicated” tissue were measured for the chemotherapy by liquid-chromatography-mass spectrometry. Complete follow-up was three months. The procedure was well-tolerated, with no adverse clinical or radiologic events related to the procedure. The BBB within the target volume showed radiographic evidence of opening with an immediate 15–50% increased contrast enhancement on T1-weighted MRI, and resolution approximately 20 hours after. Biochemical analysis of sonicated versus unsonicated tissue suggest chemotherapy delivery is feasible. In this study, we demonstrated transient BBB opening in tumor and peritumor tissue using non-invasive low-intensity MRgFUS with systemically administered chemotherapy was safe and feasible. The characterization of therapeutic delivery and clinical response to this treatment paradigm requires further investigation.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Clinical trial of blood-brain barrier disruption by pulsed ultrasound.
- Record: found
- Abstract: found
- Article: not found
The blood-brain barrier and cancer: transporters, treatment, and Trojan horses.
- Record: found
- Abstract: found
- Article: not found